OVERVIEW OF THE UPPER LIMBS
The function of the upper limb is to place the hand in position to be effective as a grasping tool. As such, the upper limb has adapted into a
body part with great freedom of motion. Muscles that control this motion extend across the back and thorax. You will review the superficial group
of back muscles which were dissected during the first block.
PROSECTION ASSIGNMENT: SUPERFICIAL VEINS AND CUTANEOUS NERVES OF THE UPPER LIMBS
Upon completion of this session, the student will be able to:
- dentify and demonstrate the areas of distribution of the major cutaneous nerves of the upper limb.
- Identify and demonstrate the major superficial veins of the upper limb.
Overview
The functional requirements of the upper limb are grasping and manipulating. As such, it is constructed for mobility at the cost of strength
and stability. The upper limb is divided into four parts: shoulder, arm (between the shoulder and elbow), forearm (between the elbow and the wrist),
and hand. It should be emphasized that the term arm refers only to the portion of the upper limb between the shoulder and the elbow, not to the
entire upper limb.
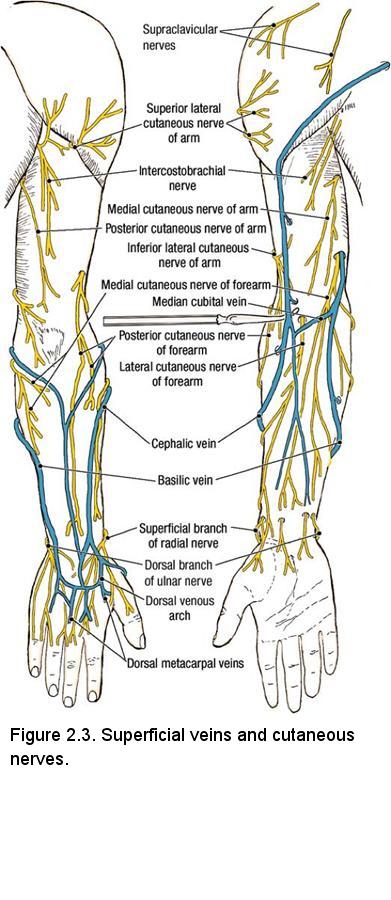
The superficial fascia of the upper limb contains fat, superficial veins, and cutaneous nerves. In the living body, the superficial veins may be visible through the skin. They are frequently used for drawing blood and injecting medications. In the cadaver, the superficial veins are not conspicuous. The cutaneous nerves of the upper limb pierce the deep fascia to reach the superficial fascia and skin.
Instructions: Superficial Veins
- Identify the cubital fossa (Figure 2.3). The cubital fossa is the depression on the anterior side of the elbow.
- Palpate the round tendon running longitudinally down the midline of the cubital fossa. This is the biceps brachii tendon.
- In the posterior forearm, identify the basilic vein and cephalic vein.
- Follow the cephalic and basilic veins proximally.
- Demonstrate that the cephalic and basilic veins are joined across the cubital fossa by the median cubital vein. This pattern can be quite variable and should be observed on other cadavers.
- Follow the cephalic vein proximally into the pectoral region where it courses in the deltopectoral groove (deltopectoral groove) between the deltoid muscle and the pectoralis major muscle. Near the clavicle, the cephalic vein passes deeply through the deltopectoral triangle to join the axillary vein.
- Follow the basilic vein proximally. Before reaching the axilla, it pierces the deep fascia to join the brachial vein.
- Use a probe to gently elevate the superficial veins (Figure 2.3). Note that perforating veins penetrate the deep fascia and connect the superficial veins to deep veins.
Instructions: Cutaneous Nerves
- Familiarize yourself with the course and distribution of the cutaneous nerves of the arm and forearm (Figure 2.3):
- Lateral cutaneous nerve of the forearm (lateral antebrachial cutaneous nerve) - located at the level of the elbow in the superficial fascia lateral to the biceps brachii tendon. Note its close relationship to the cephalic vein and the median cubital vein.
- Medial cutaneous nerve of the forearm (medial antebrachial cutaneous nerve) - located on the medial side of the biceps brachii tendon. Note its close relationship to the basilic vein.
- Superficial branch of the radial nerve - located in the superficial fascia near the styloid process of the radius (Figure 2.21). Expose only 2 or 3 cm of this nerve.
- Dorsal branch of the ulnar nerve - located in the superficial fascia near the styloid process of the ulna (Figure 2.21).
- The cutaneous nerves to the digits will be studied with the hand.
- Examine the deep fascia of the upper limb. Note that the deep fascia of the upper limb extends from the shoulder to the fingertips. It attaches to the bones of the upper limb and forms compartments that contain groups of muscles. The deep fascia of the upper limb is regionally named: brachial fascia in the arm and antebrachial fascia in the forearm. In the hand the deep fascia is called palmar fascia on the palmar surface and dorsal fascia of the hand on the dorsal surface.
Prosection Review:
- Review the superficial fascia of the upper limb.
- Use the dissected specimen to trace the course of the superficial veins from distal to proximal.
- Review the location of the cephalic vein, basilic vein, and median cubital vein in the cubital fossa and recall that these are important for venipuncture.
- Use the dissected specimen to review the four cutaneous nerves that you have dissected. Use an illustration to review the pattern of distribution of the cutaneous nerves that you did not dissect.
- Compare this pattern of cutaneous nerve distribution to a dermatome chart.
- Review the deep fascia of the upper limb and name its parts.
.jpg)
PROSECTION ASSIGNMENT: THE SHOULDER JOINT
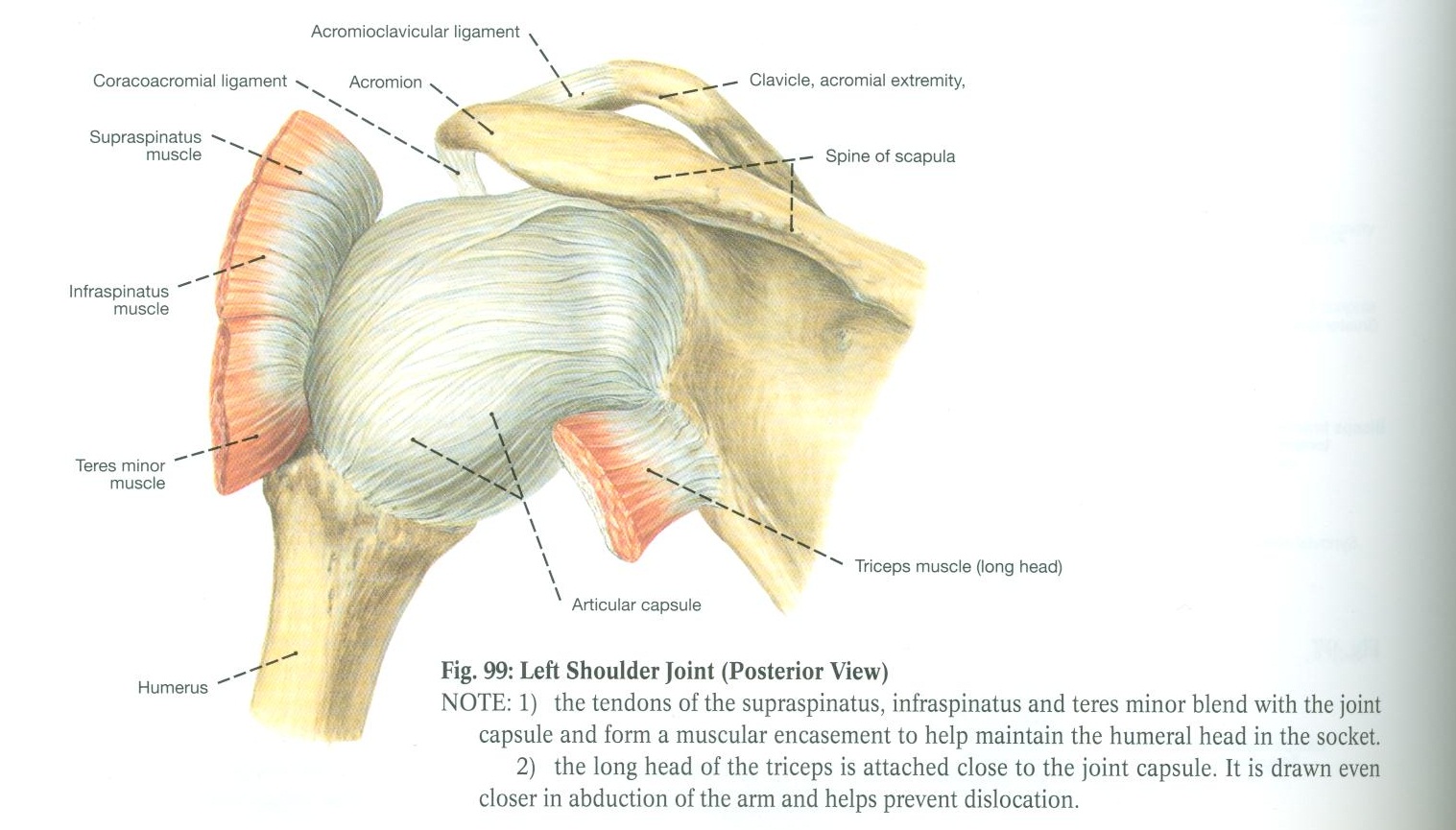
The shoulder joint consists of two bony articulations: the acromioclavicular joint and the glenohumeral joint
Acromioclavicular joint
- Review the bones that are relevant to the acromioclavicular joint:
- Acromion
- Coracoid process of the scapula
- Lateral end of the clavicle
- Identify the capsule of the acromioclavicular joint. The angle of the articulating surfaces of the acromion and clavicle causes the acromion to move inferior to the distal end of the clavicle when the acromion is forced medially.
- Identify the coracoclavicular ligament (Figure 98), which supports the acromioclavicular joint. It consists of two parts but you need not identify them. The coracoclavicular ligaments prevent the acromion from moving inferiorly relative to the clavicle, thus strengthening the acromioclavicular joint.
Glenohumeral joint (shoulder joint)
- Review the bony features pertinent to the Glenohumeral joint:
- Glenoid fossa of the scapula
- Head of the humerus
- Anatomical neck of the humerus
- Greater tubercle of the humerus
- Lesser tubercle of the humerus
- Identify the thin fibrous articular capsule of the glenohumeral joint (Figure 99)
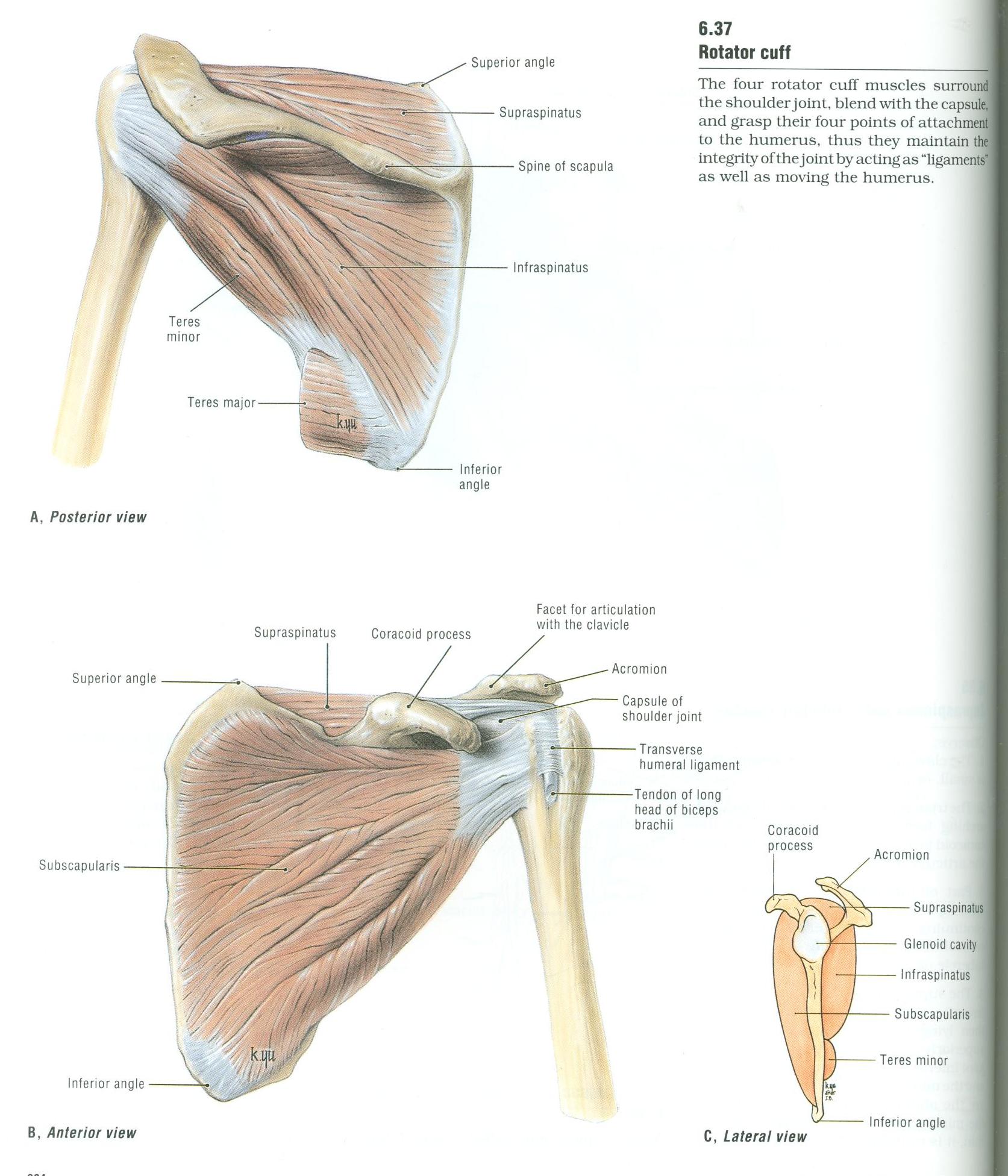
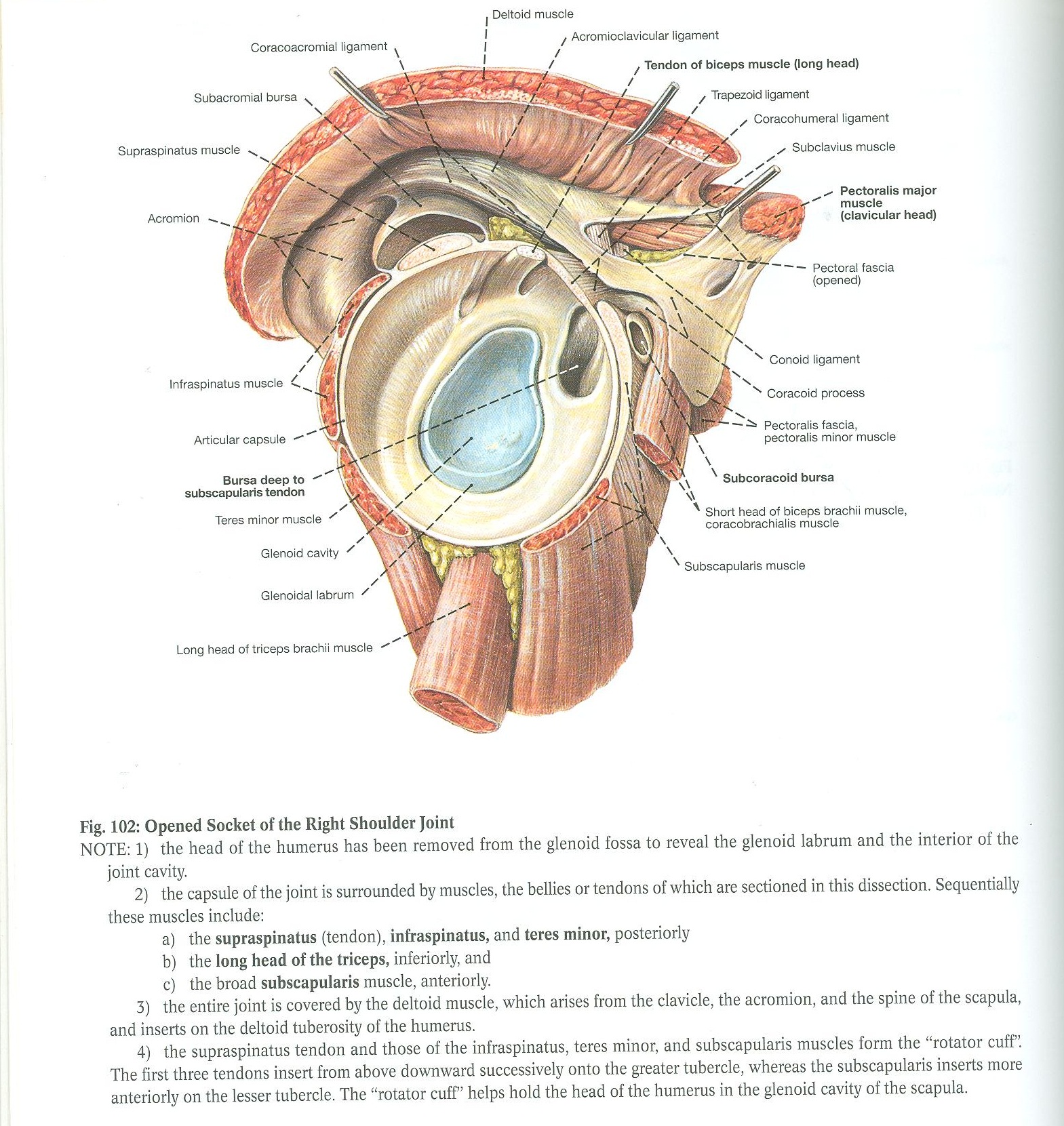
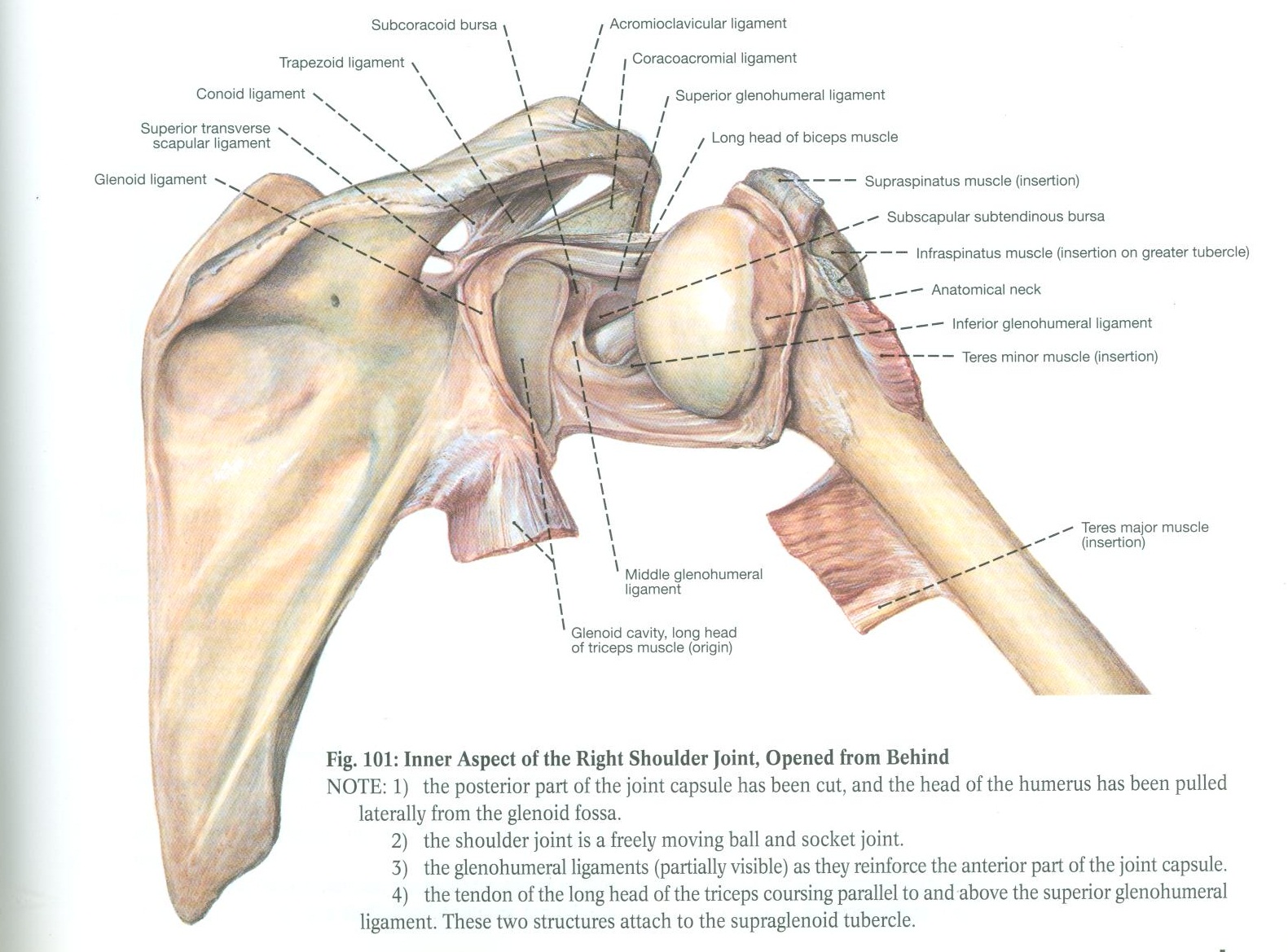
- The four rotator cuff muscles surround the shoulder joint and blend with the capsule. Identify the rotator cuff muscles: (Figure 6.37, Figure 102)
- Subscapularis muscle attaches to the lesser tubercle of the humerus and medially rotates the humerus
- Supraspinatus muscle attaches to the greater tubercle of the humerus and initiates abduction of the arm. Its tendon of insertion may be difficult to see as it is hidden below the coracoacromial ligament
- Infraspinatus muscle and teres minor muscle attach to the greater tubercle of the humerus and laterally rotate the humerus
- Identify the coracoacromial ligament. The coracoacromial ligament, the acromion and the coracoid process prevent the superior displacement of the head of the humerus
- On the prosection where the joint capsule has been opened, identify the following: (Figure 101, Figure 102)
- Glenoid fossa and glenoid labrum
- Head of the humerus covered with articular cartilage
- Anatomical neck of the humerus
- Glenohumeral ligaments are thickenings of the fibrous capsule
- Tendon of the long head of the biceps brachii muscle. It passes through the glenoid cavity and is attached to the supraglenoid tubercle.
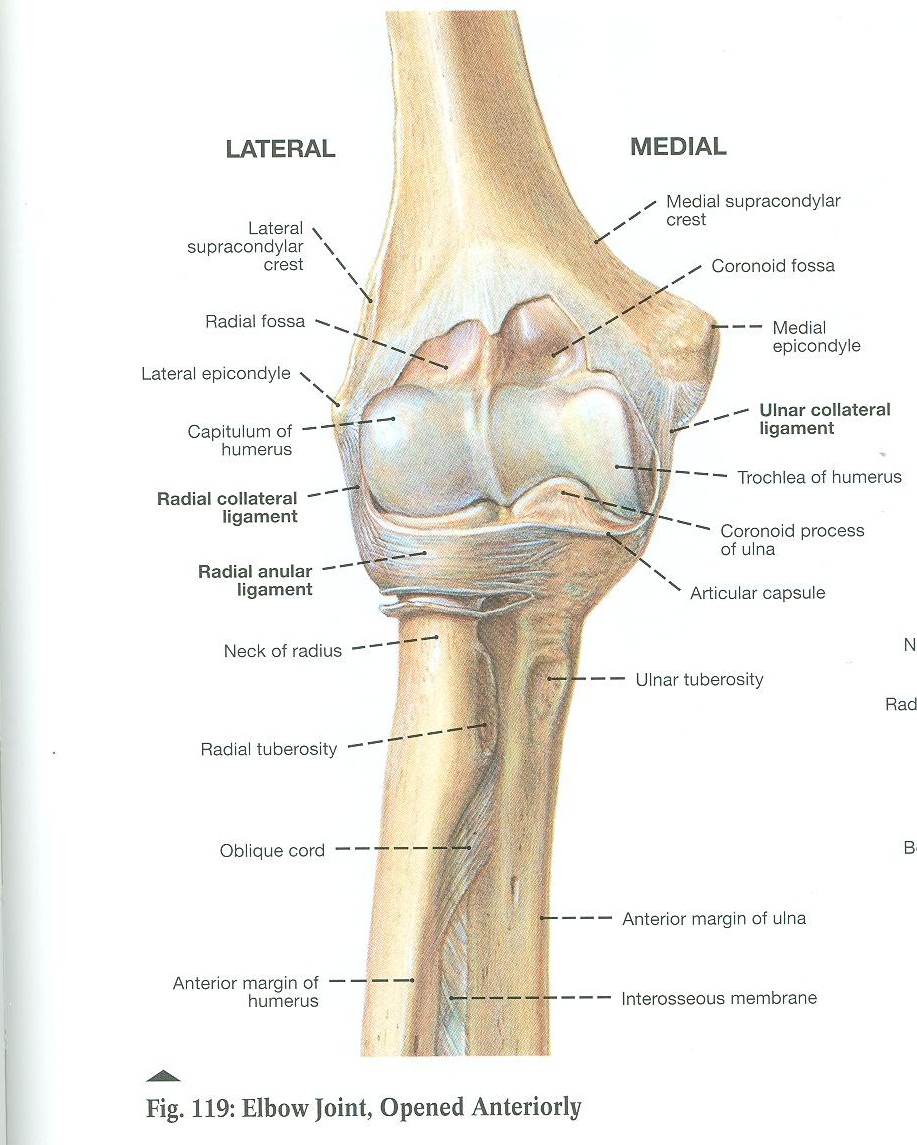
PROSECTION ASSIGNMENT: THE ELBOW JOINT
Overview: Elbow joint and proximal radioulnar joint
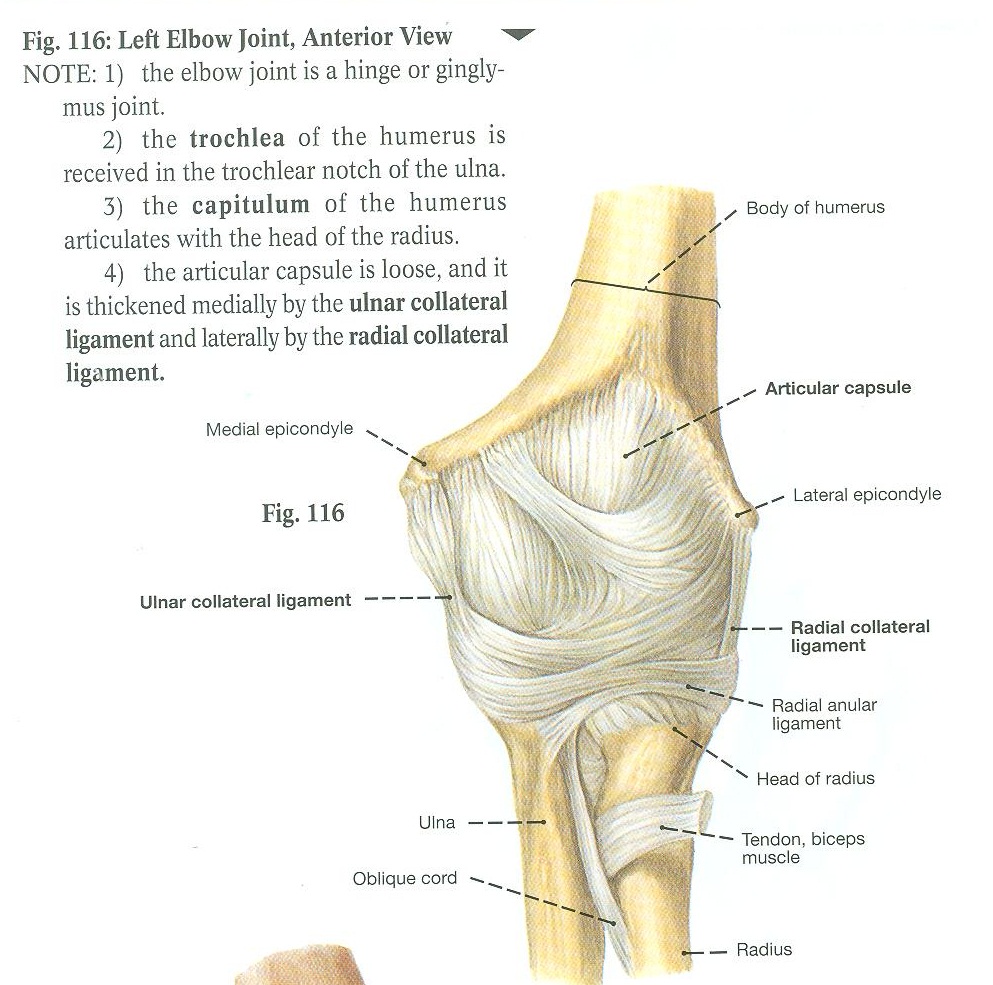
The elbow joint consists of two parts:
- A hinge joint between the trochlea of the humerus and the trochlear notch of the ulna
- A gliding joint between the capitulum of the humerus and the head of the radius
Instructions:
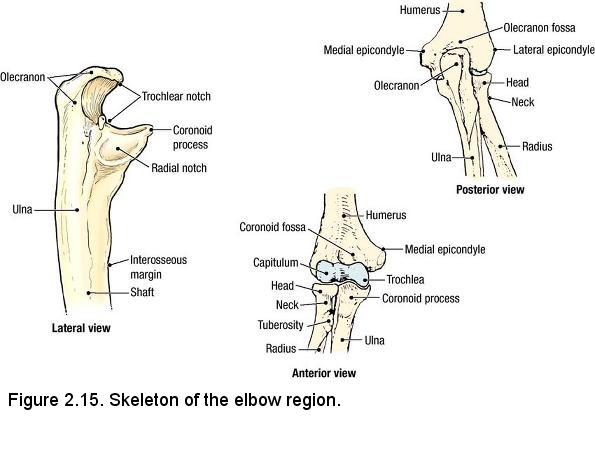
- Review the bony features of the elbow region:
- Humerus - radial fossa, coronoid fossa, lateral and medial epicondyles of the humerus, capitulum, trochlea
- Ulna - olecranon, coronoid process, radial notch
- Radius - head, neck and radial tuberosity
- Identify the thick fibrous articular capsule of the elbow joint
- Identify the ulnar collateral ligament (Figure 116). It extends from the medial epicondyle to the ulna
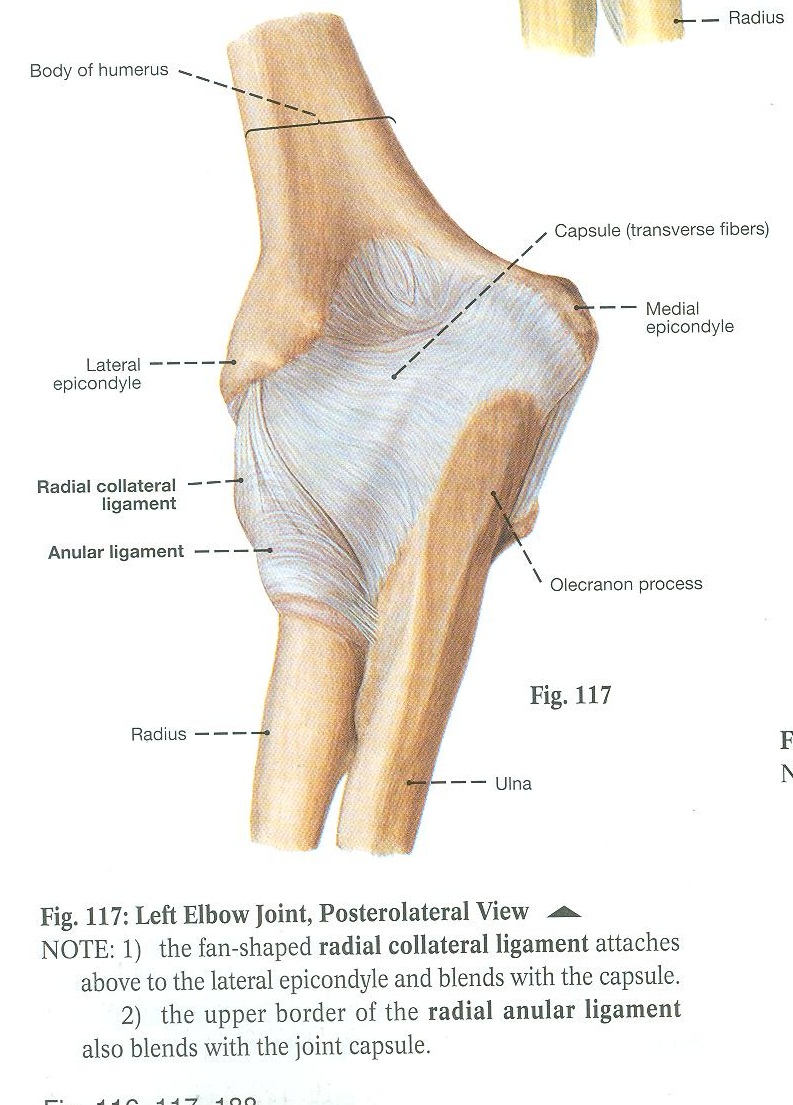
- Identify the radial collateral ligament (Figure 116, Figure 117). It extends from the lateral epicondyle to the side of the anular ligament.
- Identify the anular ligament (Figure 117, Figure 119). It is attached to both ends of the radial notch of the ulna, encircles the head of the radius and prevents it from being dislocated inferiorly. The radius can freely rotate in the anular ligament
- On the prosection where the joint has been opened anteriorly (Figure 119) identify:
- Radial fossa and coronoid fossa of the humerus
- Capitulum and trochlea of the humerus
- Coronoid process of the ulna
- Head of the radius
- Pronate and supinate the forearm and notice that the head of the radius freely rotates in the anular ligament (note that on the prosection, the supinator muscle is still present)
- Identify the interosseous membrane between the radius and the ulna.
PROSECTION ASSIGNMENT: THE WRIST JOINT
The wrist joint consists of the radiocarpal joint and the distal radioulnar joint. The radiocarpal joint is the articulation between the distal
end of the radius and the proximal carpal bones namely the scaphoid and lunate. The movements permitted at this joint are flexion, extension,
adduction and abduction. The scaphoid and lunate bones transmit forces from the hand to the forearm and thus are most commonly fractured in a
fall on the outstretched hand. The distal radioulnar joint is a pivot joint between the head of the ulna and the ulnar notch on the radius.
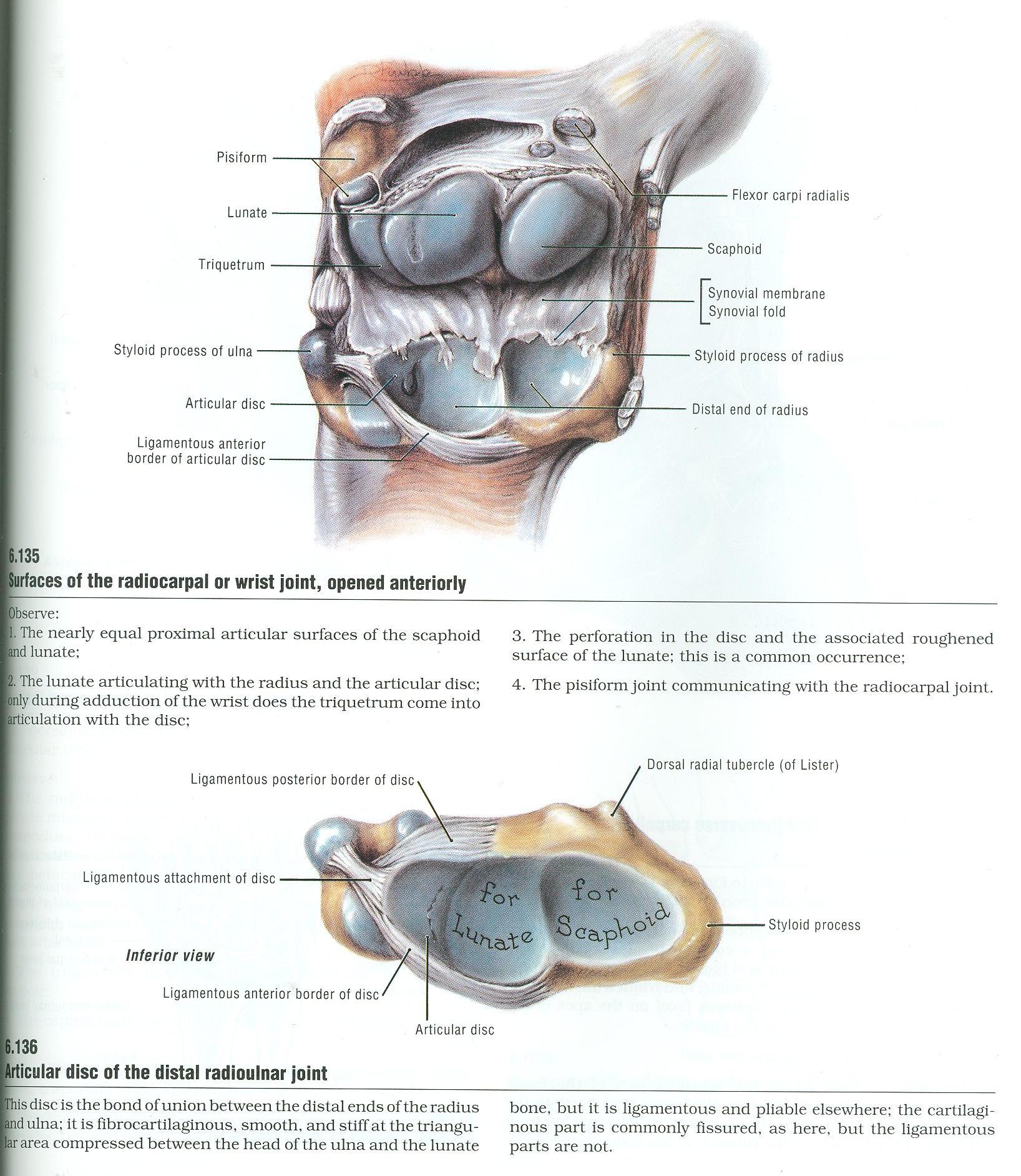
- Review the bony features of the wrist region:
- Articular surfaces of the distal end of the radius
- Articular surfaces of the head of the ulna
- Carpal bones - scaphoid and lunate
- The wrist is reinforced by
- Radiocarpal ligaments
- Radial and ulnar collateral ligaments
- On the prosection where the radiocarpal joint has been opened posteriorly, identify: (Figure 6.135-6.136)
- Articular surface on the radius for the scaphoid bone
- Articular surface on the radius for the lunate bone
- Articular surface of the scaphoid bone
- Articular surface of the lunate bone
- Articular disc of the distal radioulnar joint. The disc holds the distal ends of the radius and ulna together and separates the cavity of the distal radioulnar joint from the radiocarpal (wrist) joint.
DISSECTION LABORATORY #1: PECTORAL REGION AND AXILLA
Learning Objectives: Upon completion of this laboratory, the student will be able to:
- Identify the muscles of the pectoral region, their related fascia, nerve, regional blood supply, and general actions.
- Describe the lymphatic drainage of the upper limb and the major lymphatic node groups of the axilla.
- Recall the concept of the axilla as a space, its boundaries and its contents.
- Illustrate or describe the brachial plexus, including its parts, the nerves arising from it, and their specific origins and areas of distribution.
- Predict the functional and cutaneous loss that might result in the back, posterior shoulder, pectoral region, or cutaneous upper limb, given an injury to a specific site in the brachial plexus.
- Predict where the brachial plexus might be injured, given a functional or cutaneous loss in the back, posterior shoulder, pectoral region or cutaneous upper limb.
- Identify or describe the axillary artery and vein, their major branches, and their relationships to each other, the brachial plexus, and the pectoralis minor muscle.
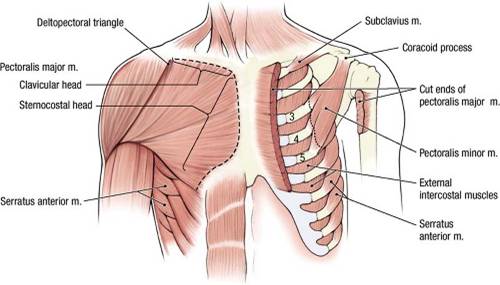
Overview: Pectoral Muscles
The pectoral region (L. pectus, chest) covers the anterior thoracic wall and part of the lateral thoracic wall. The pectoral muscles were
already dissected by the M2s in order to gain access to the thoracic cavity. The superficial fascia of the thorax contains the usual elements that
are common to superficial fascia in all body regions: blood vessels, lymph vessels, cutaneous nerves, and sweat glands. In addition, the superficial
fascia of the anterior thoracic wall in the female contains the mammary glands, which are highly specialized organs unique to the superficial fascia
of the thorax.
Instructions
- Place the cadaver in the supine position (face up).
- Study the superficial surface of the pectoralis major muscle, using your fingers to define its borders. Study an illustration and note that the deep fascia on the surface of the pectoralis major muscle is called pectoral fascia and that it is continuous with the axillary fascia that forms the floor of the axilla.
- Identify the two heads of the pectoralis major muscle: clavicular head and sternocostal head. Observe that the juncture of these two heads is at the sternoclavicular joint.
- Use your fingers to trace the tendon of the pectoralis major muscle to its distal attachment on the humerus. The pectoralis major muscle flexes, adducts, and medially rotates the humerus. With the humerus flexed, the pectoralis major muscle is converted to an extensor of the arm (although, unlike the latissimus dorsi muscle, the pectoralis major muscle is not capable of extending the arm beyond the anatomical position, i.e., it cannot extend the arm posterior to the midaxillary line).
- Between the clavicular head of the pectoralis major muscle and the adjacent deltoid muscle, use blunt dissection to define the borders of the deltopectoral triangle and find the cephalic vein (this may already be done). Preserve the cephalic vein in subsequent steps. Note that variation in venous structures is quite common; therefore the cephalic veins on your cadaver may be large or small, and are often not bilaterally symmetrical.
- The proximal attachment of the sternocostal head of the pectoralis major muscle is the sternum (Refer to figure, dashed line on subject's right side).
- Palpate the deep surface of the pectoralis major muscle to dissect the medial and lateral pectoral nerves and vessels. Preserve these nerves and vessels.
- The proximal attachment of the clavicular head of the pectoralis major muscle is the clavicle.
- Preserve the cephalic vein. Gently reflect the pectoralis major muscle laterally, noting that the lateral pectoral nerve and the pectoral branch of the thoracoacromial artery enter the deep surface of the clavicular head. Do NOT damage these structures.
- Deep to the pectoralis major muscle are the clavipectoral fascia, pectoralis minor muscle, and subclavius muscle.
- Identify the pectoralis minor muscle. The proximal attachment of the pectoralis minor muscle is ribs 3 to 5 near their costal cartilages (Refer to figure, dashed line on subject's left side). Its distal attachment is the coracoid process of the scapula. The pectoralis minor muscle draws the glenoid cavity of the scapula anteriorly and inferiorly.
- Note that the medial pectoral nerve pierces the pectoralis minor muscle and then enters the pectoralis major muscle, innervating both, while the lateral pectoral nerve (and the thoracoacromial artery) passes through the clavipectoral fascia superior to the pectoralis minor muscle, and thus innervates only the pectoralis major muscle. The clavipectoral fascia may have been removed already.
- Identify the subclavius muscle, which is located inferior to the clavicle. The subclavius muscle, which is attached to the clavicle and the first rib, depresses the clavicle.
- Read a description of the clavipectoral fascia and understand that it is immediately deep to the pectoralis major muscle. The clavipectoral fascia is attached to the clavicle. It passes both superficial and deep to the subclavius muscle and the pectoralis minor muscle. The clavipectoral fascia is attached to the axillary fascia inferiorly.
- Clean the cephalic vein, if necessary, where it crosses the anterior surface of the pectoralis minor tendon. The cephalic vein passes through the clavipectoral fascia medial to the pectoralis minor tendon.
- Reflect the pectoralis minor muscle superiorly. Leave the muscle attached to the coracoid process of the scapula.
- Within in the clavipectoral fascia, find and clean the thoracoacromial artery and the lateral pectoral nerve. Branches of the thoracoacromial artery include the following (you do not have to identify them):
- Acromial branch passes laterally across the coracoid process toward the acromion.
- Deltoid branch courses laterally in the deltopectoral groove between the deltoid muscle and pectoralis major muscle. The deltoid branch accompanies the cephalic vein.
- Pectoral branch passes between the pectoralis major muscle and the pectoralis minor muscle and supplies both.
- Clavicular branch courses superiorly and medially to supply the subclavius muscle.
- Note that you will NOT be required to name these branches specifically, just be able to identify the main thoracoacromial artery.
- Also note that the thoracoacromial artery, and the lateral and medial pectoral nerves, may be difficult to differentiate, especially if they are small. To make the distinction clear, dissect the thoracoacromial artery posteriorly until you see it branching from the large axillary artery. Clean out a small region of the axillary artery to positively identify it, removing any small veins that obscure the dissection field BUT PRESERVE THE CEPHALIC VEIN. Note that the lateral pectoral nerve arises from the brachial plexus of nerves (to be dissected later), and here is seen passing superior-lateral to the axillary artery.
- Along the lateral border of the pectoralis minor muscle, you may be able to identify the lateral thoracic artery. This vessel arises from the axillary artery near the origin and at right angles to the thoracoacromial artery, and passes inferiorly toward the thoracic cage. If you have trouble finding the lateral thoracic artery at this time, it will be traced from the axillary artery later.
- Identify the serratus anterior muscle. Note its extensive proximal attachment on the upper eight ribs. The distal attachment of the serratus anterior muscle is the deep surface of the scapula along the entire length of its medial border. You cannot see the distal attachment at this time. Find the innervation of the serratus anterior muscle, the long thoracic nerve, which arises from the brachial plexus and runs inferiorly on the lateral surface this muscle. Lesions of the long thoracic nerve result in winged scapula and weakness in abducting the arm above the shoulder.
Dissection Review
- Replace the pectoral muscles into their correct anatomical positions.
- Review the attachments of the pectoralis major, pectoralis minor, and subclavius muscles. Review their actions, innervations, and blood supply.
- Review the relationship of the clavipectoral fascia to the muscles, vessels, and nerves of this region.
- Be sure that you understand the role played by the clavipectoral fascia in supporting the floor of the axilla.
Dissection Overview: Axilla
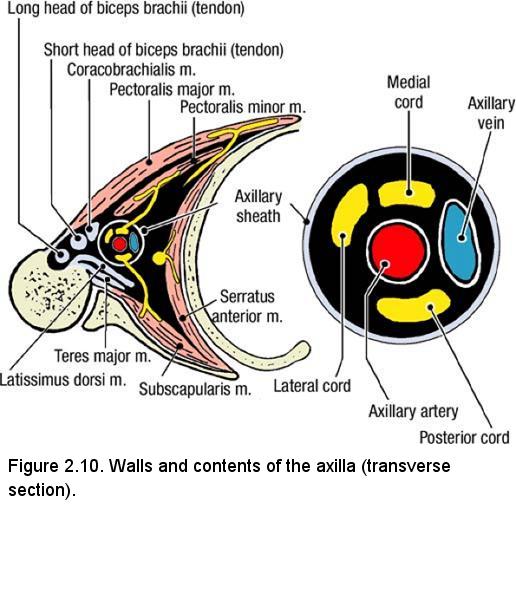
The axilla is the region between the pectoral muscles, the scapula, the arm, and the thoracic wall (Figure 2.10). It is a region of passage for
vessels and nerves that course from the root of the neck into the upper limb. The contents of the axilla are the axillary sheath, brachial plexus,
axillary artery and vein and their branches, lymph nodes and lymphatic vessels, portions of three muscles, and a considerable amount of fat and
connective tissue.
Study a diagram and note the following boundaries of the axilla:
- Apex of the axilla - bounded by the clavicle anteriorly, the upper border of the scapula posteriorly, and the first rib medially
- Base of the axilla - skin and fascia of the armpit
- Anterior wall - pectoralis major muscle, pectoralis minor muscle, and clavipectoral fascia
- Posterior wall - posterior axillary fold (teres major and latissimus dorsi muscles) and the subscapularis muscle that covers the anterior surface of the scapula
- Medial wall - upper portion of the thoracic wall and the serratus anterior muscle, which overlies this wall
- Lateral wall - intertubercular sulcus of the humerus
Dissection Instructions: Axillary Sheath
- Reflect the pectoralis major muscle laterally.
- Reflect the pectoralis minor muscle superiorly.
- Abduct the arm to about 45°.
- Identify the axillary sheath (Figure 2.10). The axillary sheath is a connective tissue structure that surrounds the axillary artery and vein, and the brachial plexus. The axillary sheath extends from the lateral border of the first rib to the inferior border of the teres major muscle.
- Use scissors to open the anterior surface of the axillary sheath.
- Identify the axillary vein within the axillary sheath. Note that the axillary vein is formed at the lateral border of the teres major muscle by the joining of the two brachial veins. The axillary vein ends at the lateral border of the first rib where it is continuous with the subclavian vein.
- To enhance dissection of the arteries and nerves in the axilla, the axillary vein must be removed. Cut the cephalic vein where it joins the axillary vein and preserve the cephalic vein. Cut the axillary vein at the lateral border of the first rib and bluntly dissect it distally as far as possible. Use a probe to dissect the axillary vein from the structures that lie posterior to it (axillary artery and brachial plexus). Cut the axillary vein at the lateral border of the teres major muscle and remove it.
- As the dissection proceeds, remove veins that are tributaries to the axillary vein. Preserve the accompanying arteries. Note the presence of lymph nodes that are associated with the veins.
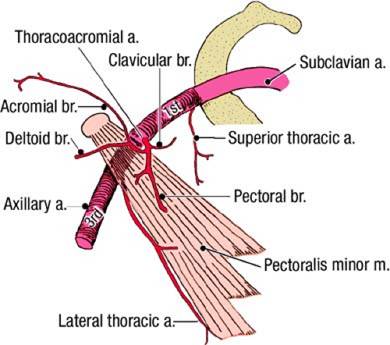
Dissection Instructions: Axillary Artery
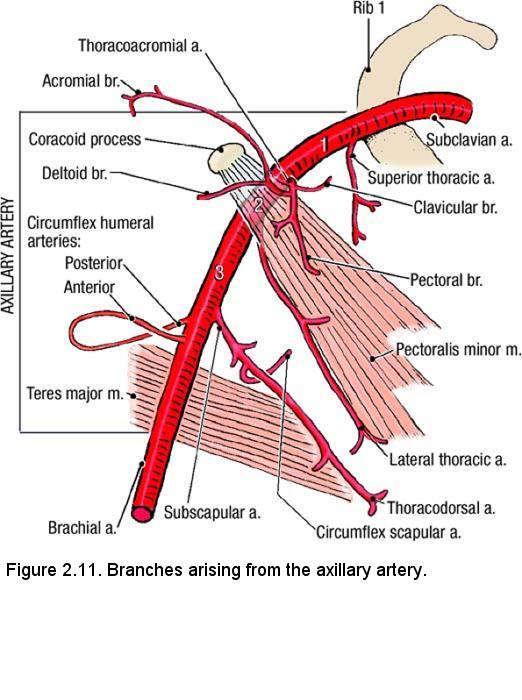
The axillary artery begins at the lateral border of the first rib where it is the continuation of the subclavian artery (Figure 2.11). The axillary
artery ends at the inferior border of the teres major muscle where its name changes to brachial artery. The axillary artery is surrounded by the
brachial plexus (Figure 2.10, inset). The brachial plexus must be retracted and preserved during dissection of the axillary artery and its branches.
- Identify the three parts of the axillary artery (Figure 2.11):
- First part extends from the lateral border of the first rib to the medial border of the pectoralis minor muscle.
- Second part lies posterior to the pectoralis minor muscle.
- Third part extends from the lateral border of the pectoralis minor muscle to the inferior border of the teres major muscle.
- Dissection note: The branching pattern of the axillary artery may vary from that which is commonly illustrated. If the pattern is different in your specimen, note that the branches are named according to their distribution rather than by their origin.
- The first part of the axillary artery has one branch, the superior thoracic artery. Follow the superior thoracic artery to its area of distribution in the first and second intercostal spaces.
- The second part of the axillary artery has two branches (Figure 2.11):
- Thoracoacromial artery arises at the medial border of the pectoralis minor muscle and penetrates the clavipectoral fascia.
- Lateral thoracic artery arises at the lateral border of the pectoralis minor muscle (65%) and descends along the lateral border of the pectoralis minor muscle. The lateral thoracic artery may arise from the subscapular artery or from the thoracoacromial artery.
- Use blunt dissection to open the clavipectoral fascia and identify the thoracoacromial artery on the medial side of the pectoralis minor muscle. The clavipectoral fascia may have already been removed to reveal the thoracoacromial artery.
- Identify the lateral thoracic artery and follow it along the lateral border of the pectoralis minor muscle (Figure 2.11). The lateral thoracic artery supplies the pectoral muscles, the serratus anterior muscle, the axillary lymph nodes, and the lateral thoracic wall. In females, the lateral thoracic artery also supplies the lateral portion of the mammary gland.
- The third part of the axillary artery has three branches: subscapular artery, posterior circumflex humeral artery, and anterior circumflex humeral artery.
- Identify the subscapular artery. It is the largest branch of the axillary artery. The subscapular artery courses inferiorly for a short distance before dividing into the circumflex scapular artery (to muscles on the posterior surface of the scapula) and the thoracodorsal artery (to the latissimus dorsi muscle). The subscapular artery gives off several unnamed muscular branches.
- Find the anterior and posterior circumflex humeral arteries, which arise from the axillary artery distal to the origin of the subscapular artery. Occasionally, these two arteries may arise from a short common trunk. They supply the deltoid muscle.
- Observe that the posterior circumflex humeral artery is the larger of the two circumflex humeral arteries. Follow it as it passes posterior to the surgical neck of the humerus with the axillary nerve. Demonstrate that the posterior circumflex humeral artery and the axillary nerve pass through the quadrangular space. The quadrangular space is bounded by the teres minor muscle, the teres major muscle, long head of the triceps brachii muscle, and the surgical neck of the humerus. The quadrangular space will be studied in more detail with scapular region.
- The anterior circumflex humeral artery courses around the anterior surface of the humerus at the surgical neck. It passes deep to the tendon of the long head of the biceps brachii muscle.
Dissection Instructions: Brachial Plexus
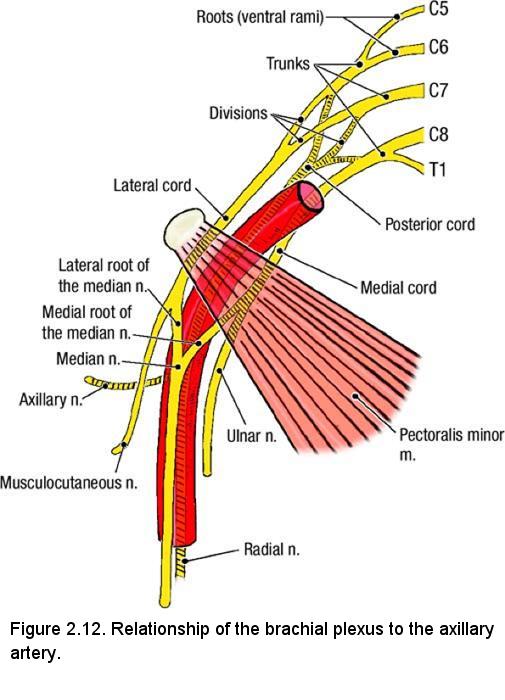
- The brachial plexus begins in the root of the neck superior to the clavicle. It passes distally toward the base of the axilla where its terminal branches arise. Only the infraclavicular part of the brachial plexus will be dissected at this time. The supraclavicular part will be dissected with the neck.
- The three cords of the brachial plexus (lateral, medial, and posterior) are named according to their relationship to the second part of the axillary artery (posterior to the pectoralis minor muscle) (Figure 2.12).
- Identify the musculocutaneous nerve. It is the most lateral terminal branch of the brachial plexus and enters the coracobrachialis muscle.
- To find the lateral cord, use your fingers to follow the musculocutaneous nerve proximally.
- Observe that the lateral cord gives rise to one other large branch, the lateral root of the median nerve. Follow the lateral root of the median nerve distally and identify the median nerve.
- To find the medial cord, trace the medial root of the median nerve proximally.
- Trace the medial cord distally to find its other terminal branch, the ulnar nerve.
- Note that the three terminal branches (musculocutaneous nerve, median nerve, and ulnar nerve) that you have just identified form the letter M anterior to the third part of the axillary artery (Figure 2.12).
- Trace the medial and lateral pectoral nerves from the reflected pectoral muscles to their origins from the medial and lateral cords, respectively.
- Identify two branches that arise from the inferior edge of the medial cord. They are the medial cutaneous nerve of the forearm (medial antebrachial cutaneous nerve) and the medial cutaneous nerve of the arm (medial brachial cutaneous nerve). Use your fingers to trace these nerves a short distance (7.5 cm) into the arm.
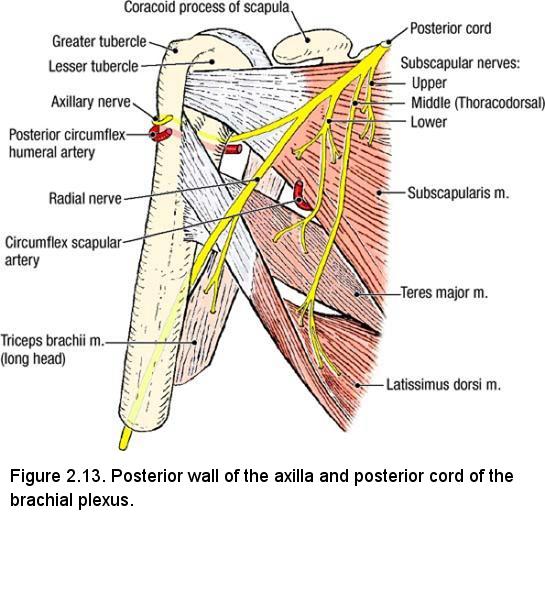
- Retract the axillary artery, the lateral cord, and the medial cord in the superior direction. This procedure exposes the posterior cord of the brachial plexus. The branches of the posterior cord are the axillary nerve, radial nerve, and three subscapular nerves (upper, middle, and lower).
- Use blunt dissection to clean the axillary nerve. Observe that the axillary nerve passes posterior to the humerus and courses through the quadrangular space with the posterior circumflex humeral artery (Figure 2.13).
- Use blunt dissection to clean the radial nerve and confirm that it leaves the axilla by passing posterior to the humerus. The radial nerve is the motor and sensory nerve to the posterior compartments of the upper limb (which we will dissect later).
- Identify the subscapular nerves that arise from the posterior cord (Figure 2.13) and verify that they run in the loose connective tissue on the anterior surface of the subscapularis muscle. Trace these nerves to their terminations:
- Upper subscapular nerve innervates the subscapularis muscle.
- Middle subscapular nerve (thoracodorsal nerve) innervates the latissimus dorsi muscle.
- Lower subscapular nerve innervates the subscapularis and the teres major muscles.
- Identify the three muscles that form the posterior wall of the axilla: latissimus dorsi, teres major, and subscapularis (Figure 2.13). Clean the anterior surfaces of these muscles.
- Examine the subscapularis muscle. The proximal attachment of the subscapularis muscle is the subscapular fossa of the scapula. The distal attachment of the subscapularis muscle is the lesser tubercle of the humerus. The subscapularis muscle medially rotates the humerus. The subscapularis muscle is a member of the rotator cuff group of muscles.
- Verify that the medial wall of the axilla is formed by the serratus anterior muscle (Figure 2.10). Use an illustration to study the attachments of the serratus anterior muscle. The proximal attachments of the serratus anterior muscle are the external surfaces of ribs 1 to 8. Its distal attachment is the anterior surface of the medial border of the scapula. The serratus anterior muscle protracts the scapula. The serratus anterior muscle also rotates the scapula, especially when the arm is abducted above the horizontal plane.
- Use your fingers to follow the serratus anterior muscle posteriorly toward the medial margin of the scapula. On the superficial surface of this muscle, use a probe to free the long thoracic nerve. Note the vertical course of this nerve. Observe its branches to the serratus anterior muscle. Follow the nerve superiorly as far as possible toward the apex of the axilla.
IN THE CLINIC: Nerve Injuries
The long thoracic nerve is vulnerable to stab wounds and to surgical injury during radical mastectomy. Injury of the long thoracic nerve affects the serratus anterior muscle. When a patient with paralysis of the serratus anterior muscle is asked to push with both hands against a wall, the medial border of the scapula protrudes on the affected side, a condition known as "winged scapula."
The thoracodorsal nerve is vulnerable to compression injuries and surgical trauma during mastectomy. Injury of the thoracodorsal nerve affects the latissimus dorsi muscle resulting in a weakened ability to extend, adduct, and medially rotate the arm.
The axillary nerve courses around the surgical neck of the humerus and may be injured during a fracture or during an inferior dislocation of the shoulder joint. Injury of the axillary nerve affects the deltoid muscle and teres minor muscle, resulting in a weakened ability to abduct and laterally rotate the arm.
The long thoracic nerve is vulnerable to stab wounds and to surgical injury during radical mastectomy. Injury of the long thoracic nerve affects the serratus anterior muscle. When a patient with paralysis of the serratus anterior muscle is asked to push with both hands against a wall, the medial border of the scapula protrudes on the affected side, a condition known as "winged scapula."
The thoracodorsal nerve is vulnerable to compression injuries and surgical trauma during mastectomy. Injury of the thoracodorsal nerve affects the latissimus dorsi muscle resulting in a weakened ability to extend, adduct, and medially rotate the arm.
The axillary nerve courses around the surgical neck of the humerus and may be injured during a fracture or during an inferior dislocation of the shoulder joint. Injury of the axillary nerve affects the deltoid muscle and teres minor muscle, resulting in a weakened ability to abduct and laterally rotate the arm.
Dissection Review
- Replace the pectoralis major muscle and the pectoralis minor muscle into their correct anatomical positions and review their attachments.
- Review the boundaries of the axilla.
- Use the dissected specimen to observe the relationship of the three parts of the axillary artery to the pectoralis minor muscle.
- Recite the names of all of the branches of the axillary artery and identify each branch on your dissected specimen.
- Test your understanding of the brachial plexus by drawing a picture that shows its structure and branches. Extend this exercise to the cadaver by demonstrating the divisions, cords, and terminal branches of the infraclavicular portion of the brachial plexus.
- Review the motor nerve supply to the muscles of the scapular region. Name each muscle and the nerve that supplies it. Realize that some of these nerves arise from the supraclavicular portion of the brachial plexus and that they have not yet been dissected completely.
- Review the movements of the scapula.
- Examine other cadavers to gain an appreciation of variations in the branching patterns of arteries and nerves.
- Use an illustration to review the lymphatic drainage of the axilla.
DISSECTION LABORATORY #2: ANTERIOR ARM, CUBITAL FOSSA, AND THE ANTERIOR FOREARM
Upon completion of this session, the student will be able to:
- Identify prominent features of the humerus, cubital fossa and associated prominences of the scapula, radius and ulna as given in the lab manual.
- Identify the contents of the anterior compartment of the arm and the functional significance of the included muscles.
- Correlate any fractures of the humerus with functional disruptions of associated muscular and neurovascular structures.
- Describe the movements of the shoulder and elbow joints.
- Identify spatial relationships of all associated muscular and neurovascular structures within the cubital fossa.
- Identify the prominent features of the humerus, ulna, radius, carpals, metacarpals and phalanges.
- Identify the flexor compartment of the forearm, the nerve and vessels supplying its contents, and the functional significance of the included muscles.
- Correlate any fractures or deep cuts of the forearm with functional disruptions of associated muscular or neurovascular structures.
- Describe the movements of elbow, wrist, and finger joints.
Osteology of the Arm
- Medial epicondyle
- Lateral epicondyle
- Olecranon fossa
On the radius, identify:
- Head
- Neck
- Tuberosity
On the ulna, identify:
- Olecranon
- Coronoid process
Dissection Instructions: Anterior Compartment of the Arm
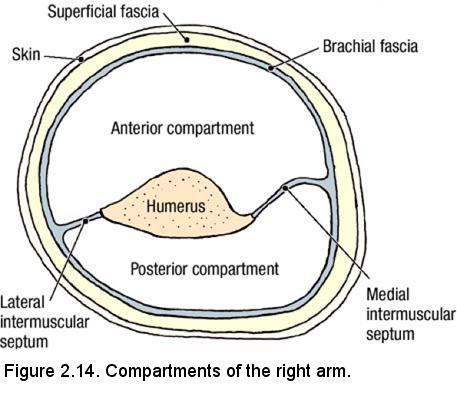
The brachial fascia (deep fascia of the arm) is a sleeve of tough connective tissue that is continuous at its proximal end with the pectoral fascia,
the axillary fascia, and the deep fascia that covers the deltoid and latissimus dorsi muscles. Distally, the brachial fascia is continuous with the
antebrachial fascia (deep fascia of the forearm). The brachial fascia is connected to the medial and lateral sides of the humerus by intermuscular
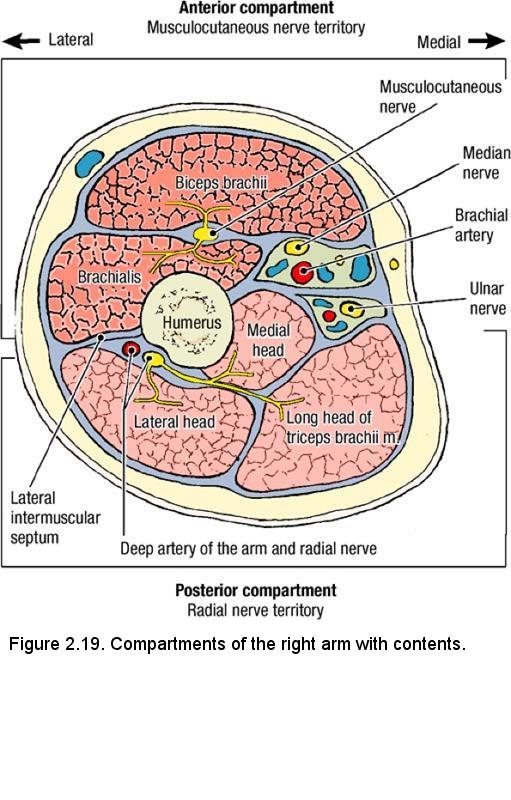
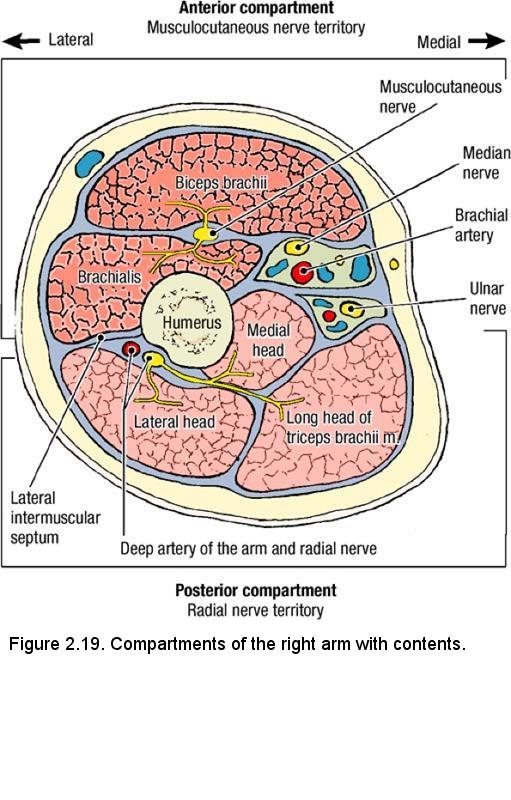
septa (Figure 2.14), creating an anterior (flexor) compartment and a posterior (extensor) compartment for the muscles of the arm. The anterior
compartment contains three muscles (biceps brachii, brachialis, and coracobrachialis) and the musculocutaneous nerve. The posterior compartment
contains two muscles (triceps brachii and anconeus), the radial nerve, and the deep artery and vein of the arm. The posterior compartment will be
dissected later.
The order of dissection will be as follows: The anterior compartment of the arm will be opened and its contents will be studied. Nerves and blood vessels will then be traced distally through the arm to the elbow region.
- Place the cadaver in the supine position.
- Begin by observing the previously dissected brachial plexus. In particular, note that the anterior distal branches of the brachial plexus typically form the shape of an M. The lateral nerve of the M is the musculocutaneous nerve, the middle stem is the median nerve, and the medial branch is the ulnar nerve.
- Use scissors to make a longitudinal incision in the anterior surface of the brachial fascia from the level of the pectoralis major tendon to the elbow.
- Use your fingers to separate the brachial fascia from the underlying muscles. Work laterally and medially from the incision and note the presence of the lateral intermuscular septum and the medial intermuscular septum.
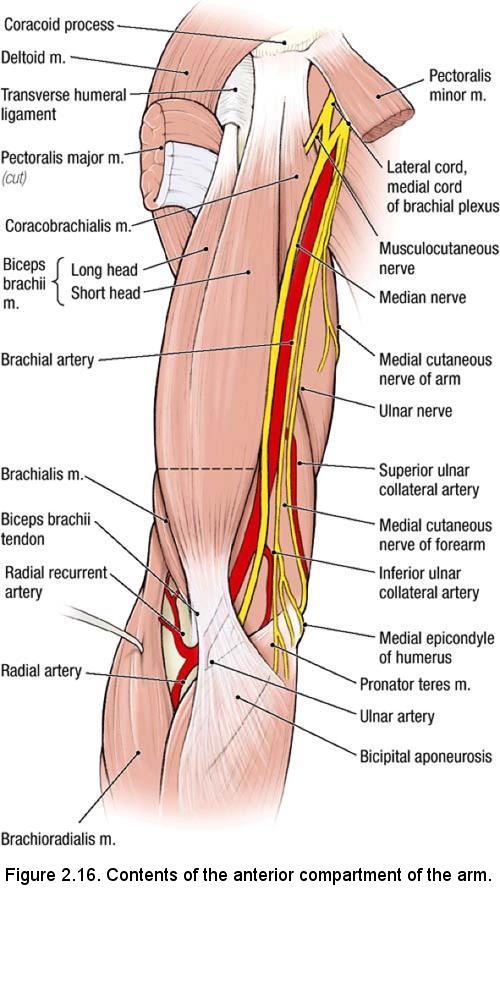
- Use your fingers to separate the three muscles in the anterior compartment of the arm: coracobrachialis, brachialis, and biceps brachii (Figure 2.16).
- The biceps brachii muscle has two proximal attachments on the scapula:
- Short head of the biceps brachii muscle attaches to the coracoid process of the scapula.
- Long head of the biceps brachii muscle attaches to the supraglenoid tubercle of the scapula.
- The tendon of the long head of the biceps brachii muscle courses through the intertubercular sulcus of the humerus (bicipital groove) posterior to the transverse humeral ligament, then enters the shoulder joint. Do not follow the tendon of the long head to its attachment on the scapula.
- Identify the biceps brachii tendon at the level of the elbow (Figure 2.16). The distal attachment of the biceps brachii muscle is on the radial tuberosity. The biceps brachii muscle supinates and flexes the forearm.
- Identify the bicipital aponeurosis (Figure 2.16). The bicipital aponeurosis is a broad extension of the biceps brachii tendon that attaches to the antebrachial fascia. The bicipital aponeurosis is located on the medial side of the biceps brachii tendon.
- Find the musculocutaneous nerve in the axilla (Figure 2.16). Follow the musculocutaneous nerve distally until it enters the coracobrachialis muscle. Note that the musculocutaneous nerve innervates the three muscles of the anterior compartment of the arm.
- Use your fingers to confirm that the proximal attachment of the coracobrachialis muscle is the coracoid process and that its distal attachment is on the medial side of the shaft of the humerus. The coracobrachialis muscle adducts and flexes the humerus.
- Use scissors to transect the biceps brachii muscle about 5 cm proximal to the elbow (Figure 2.16, dashed line). Preserve the musculocutaneous nerve. Reflect the two portions of the biceps brachii muscle proximally and distally, respectively.
- Observe the brachialis muscle, which is deep to the biceps brachii muscle. The proximal attachment of the brachialis muscle is the anterior surface of the humerus and its distal attachment is on the coronoid process of the ulna. The brachialis muscle flexes the forearm.
- Find the musculocutaneous nerve where it emerges from the coracobrachialis muscle. Follow the musculocutaneous nerve through the plane of loose connective tissue between the biceps brachii muscle and brachialis muscle.
- After the musculocutaneous nerve gives off its muscular branches, it continues distally as the lateral cutaneous nerve of the forearm (lateral antebrachial cutaneous nerve). Follow the lateral cutaneous nerve of the forearm to the cubital fossa where it emerges near the lateral side of the biceps brachii tendon. Review the relationship of the lateral cutaneous nerve of the forearm to the cephalic vein.
- Follow the medial cutaneous nerve of the forearm from the brachial plexus to the level of the elbow (Figure 2.16). Note its relationship to the basilic vein at the level of the elbow.
- Find the median nerve where it arises from the brachial plexus (Figure 2.16). Use blunt dissection to follow the median nerve from the axilla to the cubital fossa. The median nerve courses distally within the medial intermuscular septum.
- Use blunt dissection to follow the ulnar nerve from the medial cord of the brachial plexus to the medial epicondyle of the humerus (Figure 2.16). Note that the ulnar nerve is in contact with the posterior surface of the medial epicondyle of the humerus, where it is covered by only skin and a thin layer of subcutaneous fascia. Palpate the ulnar nerve on yourself where it passes posterior to the medial epicondyle. Mild trauma to the ulnar nerve at this location is what is commonly referred to as the "funny bone".
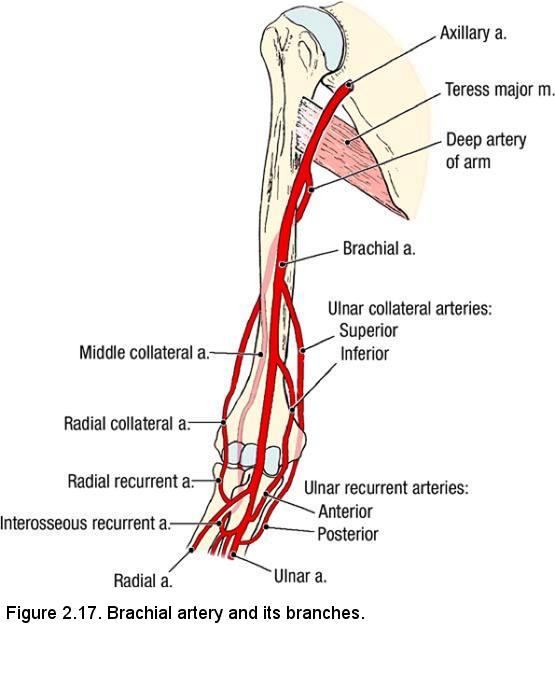
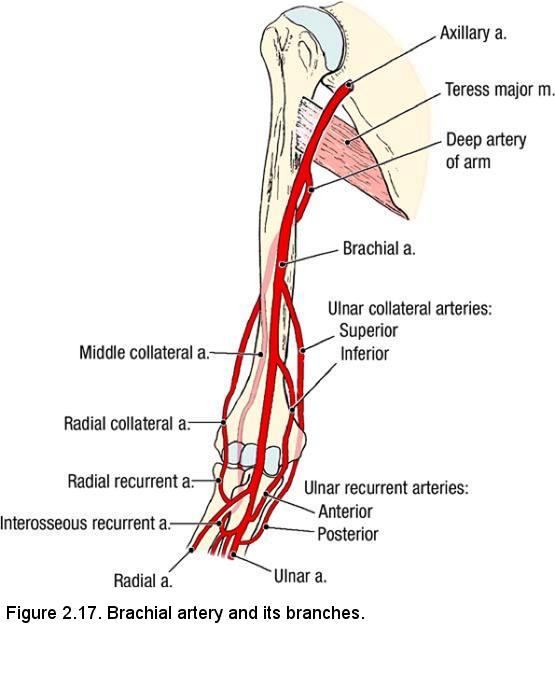
- Identify the brachial artery. The brachial artery is the continuation of the axillary artery. The brachial artery begins at the inferior border of the teres major muscle and ends at the level of the elbow by branching into the ulnar artery and radial artery (Figure 2.16). Verify that the brachial artery courses with the median nerve within the medial intermuscular septum, and that the median nerve is the only large structure to cross the anterior surface of the brachial artery.
- The brachial artery has three named branches in the arm: deep artery of the arm, superior ulnar collateral artery, and inferior ulnar collateral artery. Several unnamed muscular branches also arise along the length of the brachial artery.
- Remove the brachial veins and their tributaries to clear the dissection field. Preserve the branches of the brachial artery.
- In the proximal arm, find the deep artery of the arm (deep brachial artery, profunda brachii artery) where it arises from the brachial artery (Figure 2.17). The deep artery of the arm courses around the posterior surface of the humerus, where it accompanies the radial nerve in the radial groove. The course of the deep artery of the arm will be seen when the posterior compartment of the arm is dissected.
IN THE CLINIC: Brachial Artery
Use an illustration to study the collateral circulation around the elbow joint (Figure 2.17). The brachial artery may become blocked at any level distal to the deep artery of the arm without completely blocking blood flow to the forearm and hand.
In the arm, the brachial artery lies medial to the biceps brachii muscle and close to the shaft of the humerus. The brachial artery is compressed at this location when taking a blood pressure reading.
Use an illustration to study the collateral circulation around the elbow joint (Figure 2.17). The brachial artery may become blocked at any level distal to the deep artery of the arm without completely blocking blood flow to the forearm and hand.
In the arm, the brachial artery lies medial to the biceps brachii muscle and close to the shaft of the humerus. The brachial artery is compressed at this location when taking a blood pressure reading.
Dissection Instructions: Cubital Fossa
The cubital fossa (L. cubitus, elbow) is the depression on the anterior aspect of the elbow. The cubital fossa is clinically important
because it contains superficial veins that are used for venipuncture. Large nerves and vessels pass through this region to enter the forearm.
- Note the boundaries of the cubital fossa (Figure 2.16):
- Lateral boundary - brachioradialis muscle
- Medial boundary - pronator teres muscle
- Superior boundary - an imaginary line connecting the medial and lateral epicondyles of the humerus
- Superficial boundary (roof of the cubital fossa) - antebrachial fascia reinforced by the bicipital aponeurosis
- Deep boundary (floor of the cubital fossa) - brachialis and supinator muscles
- Review the positions of the cephalic vein, basilic vein, and median cubital vein in the cubital fossa. To gain access to deeper structures it may be necessary to cut the median cubital vein and retract its cut ends medially and laterally, respectively.
- Find the tendon of the biceps brachii muscle in the cubital fossa.
- Cut the bicipital aponeurosis near the biceps brachii tendon and reflect the bicipital aponeurosis medially. Do not cut the brachial artery, which lies deep to the bicipital aponeurosis.
- Follow the median nerve and the brachial artery from the arm into the cubital fossa. Remove any fat that may be obstructing your view of these structures.
- Observe the relative positions of the structures in the cubital fossa (Figure 2.16): The biceps brachii tendon is lateral, the brachial artery is intermediate, and the median nerve is medial (TAN = Tendon, Artery, Nerve). Note that the bicipital aponeurosis passes superficial to the brachial artery and median nerve, but it lies deep to the superficial veins. The bicipital aponeurosis protects the brachial artery and median nerve from injury during venipuncture.
Dissection Review
- Replace the muscles of the anterior compartment of the arm in their correct anatomical positions.
- Review the proximal attachment, distal attachment, nerve, and action of each muscle.
- Use the dissected specimen to review the origin, course, termination, and branches of the brachial artery.
- Trace each nerve that you have dissected from the brachial plexus to the elbow, reviewing relationships.
- Review a drawing of a cross section of the arm and notice the position of the brachial fascia and the intermuscular septa relative to the structures that you have dissected.
- Review the nerve territories of the brachial region (Figure 2.19).
- Recall the rules of innervation of the muscles of the arm:
- All muscles in the anterior compartment of the arm are innervated by the musculocutaneous nerve
- All muscles in the posterior compartment of the arm are innervated by the radial nerve (we will study these muscles and follow the radial nerve into the posterior compartment in a later lab).
- The median nerve and the ulnar nerve do not innervate muscles in the arm.
Osteology of the Forearm
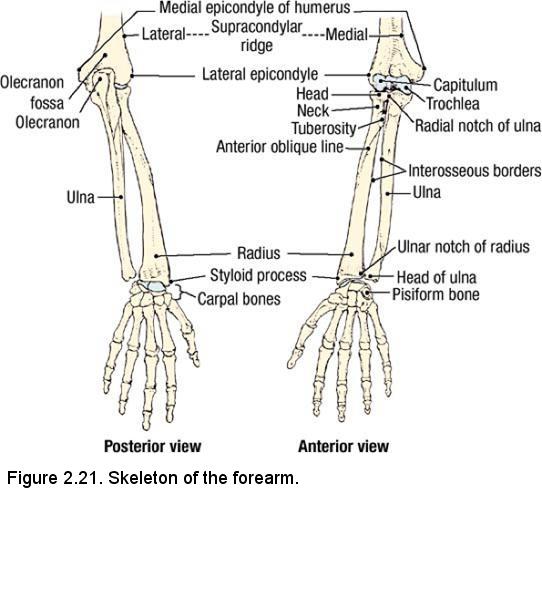
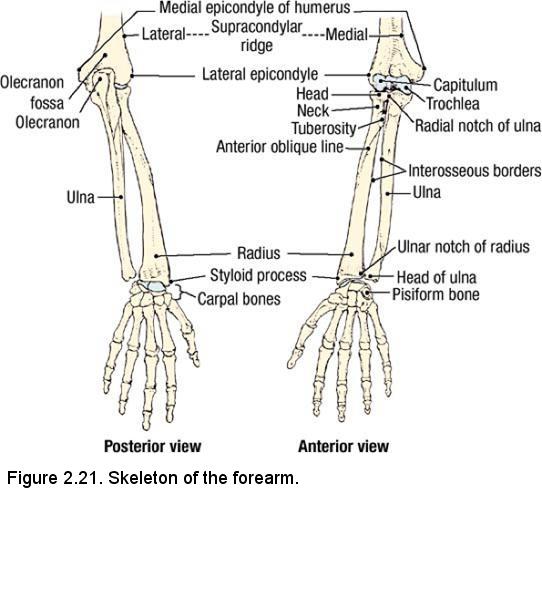
Refer to the skeleton of the forearm. On the humerus, identify (Figure 2.21):
- Medial epicondyle
- Medial supracondylar ridge
- Lateral epicondyle
- Lateral supracondylar ridge
- Capitulum
- Trochlea
- Olecranon fossa
On the radius, identify (Figure 2.21):
- Head
- Neck
- Tuberosity
- Anterior oblique line
- Ulnar notch
- Styloid process
- Interosseous border for attachment of the interosseous membrane
On the ulna, identify (Figure 2.21):
- Olecranon
- Trochlear notch
- Radial notch
- Head
- Interosseous border for attachment of the interosseous membrane
On the skeleton, examine the elbow joint. The elbow joint is the articulation between the trochlear notch of the ulna and the trochlea of the humerus, and the articulation between the
Observe the proximal radioulnar joint between the head of the radius and the radial notch of the ulna. Observe the distal radioulnar joint between the head of the ulna and the ulnar notch of the radius. Pronate and supinate the hand of the skeleton and notice the rotational movements that occur in the proximal and distal radioulnar joints. In the position of supination (anatomical position), the radius and the ulna are parallel. In the position of pronation, the radius crosses the ulna.
Dissection Overview: Anterior Compartment of the Forearm
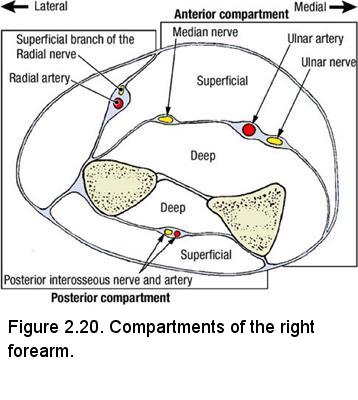
The antebrachial fascia is a sleeve of connective tissue that invests the forearm. Intermuscular septa project inward from it and attach the
antebrachial fascia to the radius and ulna (Figure 2.20). The intermuscular septa, the interosseous membrane, the radius, and the ulna combine to
divide the forearm into an anterior (flexor) compartment and a posterior (extensor) compartment.
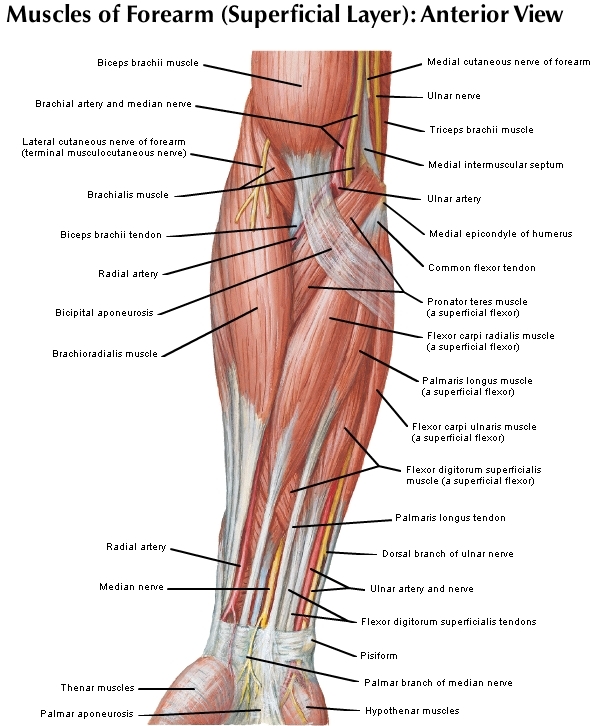
The muscles in the anterior compartment of the forearm can be divided into a superficial group of flexor muscles and a deep group of flexor muscles. Muscles of the superficial flexor group arise primarily from the medial epicondyle of the humerus and its supracondylar ridge. Muscles of the deep flexor group arise from the anterior surfaces of the radius, ulna, and interosseous membrane. Study a transverse section through the midlevel of the forearm (Figure 2.20). Note that the ulnar artery, ulnar nerve, and median nerve are in a connective tissue plane that separates the superficial flexor group from the deep flexor group.
The order of dissection will be as follows: The structures in the superficial fascia will be reviewed and the antebrachial fascia will be removed. At the level of the wrist, the relative positions of tendons, vessels, and nerves will be studied. The superficial group of flexor muscles will be studied and then reflected. Vessels and nerves that lie between the superficial and deep groups of flexor muscles will be studied. The deep group of flexor muscles will be dissected.
Dissection Instructions: Superficial Muscles of the Anterior Forearm
- Place the cadaver in the supine position and abduct the upper limb. Forcefully supinate the hand and fasten it to the board with a bungee cord to hold it in this position. When working with the bungee cords, be sure that they are securely fastened and take extra care when unfastening these cords. They are under tension and the metal hooks may fly freely with high velocity.
- Use blunt dissection to remove the remnants of the superficial fascia, taking care to preserve the cephalic and basilic veins.
- Use scissors to incise the anterior surface of the antebrachial fascia from the cubital fossa to the wrist. Use your fingers or a probe to separate the antebrachial fascia from the muscles that lie deep to it. Detach the antebrachial fascia from its attachments to the radius and ulna and place it in the tissue container.
- Use blunt dissection to clean the superficial group of flexor muscles: pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis. The flexor digitorum superficialis muscle is located deep to the other four muscles in this group. The brachioradialis muscle is a forearm flexor located on the lateral side of the anterior forearm. The brachioradialis muscle and its relationships will be described and dissected in both the flexor and extensor compartments of the forearm.
- Note that the proximal attachment of the brachioradialis muscle is the lateral surface of the distal humerus. Note that part of the proximal attachment of the pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis muscles is from a common flexor tendon. The common flexor tendon is attached to the medial epicondyle of the humerus.
- Note that the distal attachment of the brachioradialis muscle is to the styloid process of the radius.
- Note the distal attachment and action of each muscle of the superficial group of flexors:
- Pronator teres muscle attaches to the middle of the lateral surface of the radius. The pronator teres muscle pronates the hand and flexes the forearm.
- Flexor carpi radialis tendon attaches to the base of the second metacarpal bone. The flexor carpi radialis muscle flexes and abducts the hand.
- Palmaris longus tendon attaches to the palmar aponeurosis. The palmaris longus muscle flexes the hand.
- Flexor carpi ulnaris tendon attaches to the pisiform bone, the hamate bone, and the base of the fifth metacarpal bone. The flexor carpi ulnaris muscle flexes and adducts the hand.
- Flexor digitorum superficialis tendons attach to the middle phalanges of digits 2 to 5. The flexor digitorum superficialis muscle flexes the middle phalanges of digits 2 to 5.
- Use your fingers to separate the tendons of the superficial group of flexor muscles. Note that the muscle bellies cannot be easily
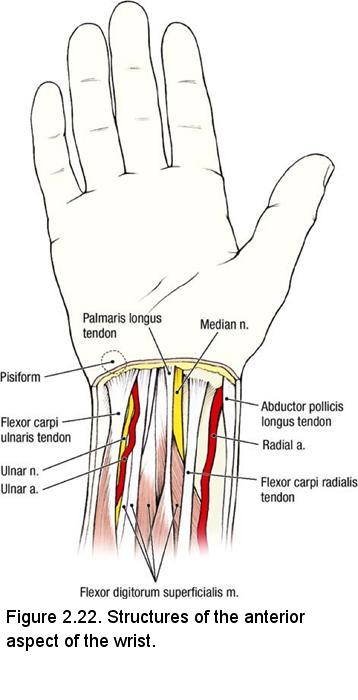
separated from each other. From lateral to medial, identify the superficial structures at the wrist (Figure 2.22):
- Tendon of the abductor pollicis longus muscle (the belly of this muscle is located in the posterior forearm)
- Radial artery
- Tendon of the flexor carpi radialis muscle
- Median nerve
- Tendon of the palmaris longus muscle (absent in 13% of limbs)
- Four tendons of the flexor digitorum superficialis muscle
- Ulnar artery and ulnar nerve
- Tendon of the flexor carpi ulnaris muscle
- Palpate the tendons listed above in your own wrist. Feel the pulse of the radial artery between the abductor pollicis longus and flexor carpi radialis tendons. The median nerve is superficial at the wrist and can be easily injured. Palpate the distal attachment of the flexor carpi ulnaris tendon on the pisiform bone. Palpate the ulnar nerve and artery, which lie immediately lateral to the pisiform bone.
Dissection Instructions: Vessels and Nerves
- At the point where the pronator teres muscle passes deep to the brachioradialis muscle, use your fingers to open the connective tissue plane that is medial to the brachioradialis muscle (DO NOT MAKE THE CUTS SHOWN IN THE FIGURE). In this intermuscular plane, identify the superficial branch of the radial nerve, which courses distally on the deep surface of the brachioradialis muscle. Trace the superficial branch of the radial nerve to the distal one-third of the forearm and confirm that it emerges on the dorsal side of the brachioradialis tendon to become a cutaneous nerve.
- Once again, identify the brachial artery in the cubital fossa. Use blunt dissection to trace the brachial artery distally until it bifurcates into the radial artery and the ulnar artery).
- Use a probe to clean the radial artery and follow it distally to the level of the wrist. The radial vein and its tributaries may be removed to clear the dissection field. The radial artery gives rise to several unnamed muscular branches in the forearm.
- Find the radial recurrent artery, which arises from the radial artery near its origin from the brachial artery. The radial recurrent artery courses proximally in the connective tissue plane between the brachioradialis muscle and the brachialis muscle. The radial recurrent artery anastomoses with the radial collateral branch of the deep artery of the arm. The radial recurrent artery is part of the anastomotic network around the elbow (Figure 2.17).
- Identify the median nerve in the cubital fossa (Figure 2.16). It is medial to the brachial artery. The median nerve innervates most (but not all) of the muscles of the flexor compartment of the forearm.
- Follow the median nerve distally. The median nerve courses deep to the superficial group of flexor muscles (Figure). To expose the
median nerve, use scissors to cut the tendon of the palmaris longus muscle about 3 cm proximal to the wrist and reflect the muscle
belly proximally. Cut the tendon of the flexor carpi radialis muscle about 5 cm proximal to the wrist and reflect it proximally.
- Insert a probe through the pronator teres muscle along the anterior surface of the median nerve. Use scissors to cut the portion of the pronator teres muscle that lies anterior to the median nerve. Use a probe to release the median nerve and follow it distally.
- Observe that the median nerve passes deep to the flexor digitorum superficialis muscle. Use scissors to detach the flexor digitorum superficialis muscle from its proximal attachment on the radius. Retract the muscle medially, leaving its ulnar and humeral attachments undisturbed.
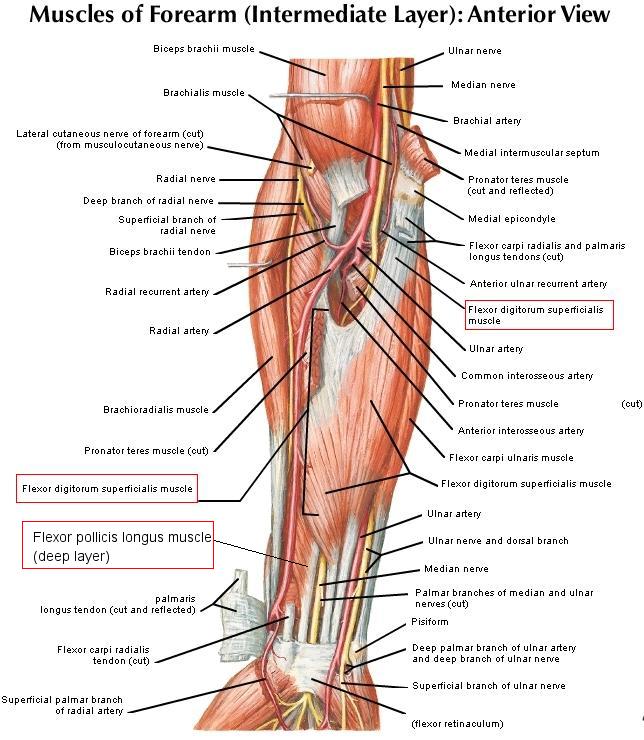
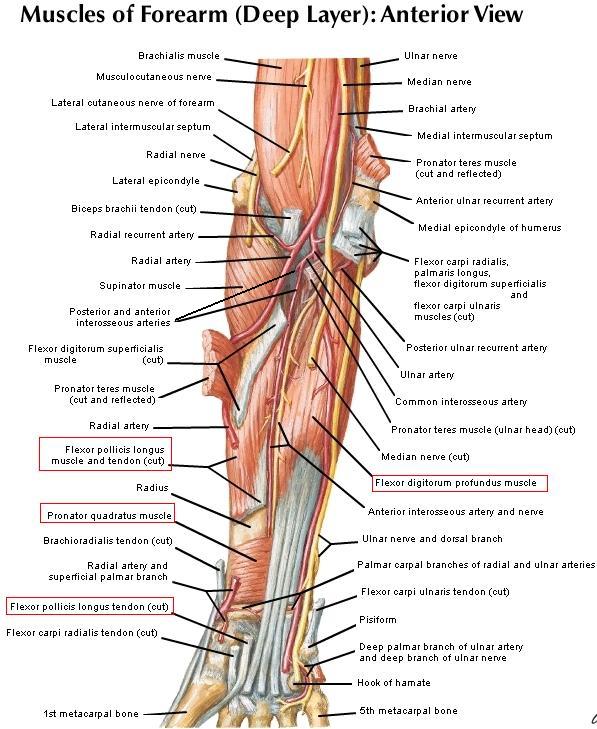
- Refer to ("Muscles of the Forearm (deep layer)" but do not make the cuts shown in the figure unless indicated in the text). Use a probe to free the median nerve from the loose connective tissue that lies between the superficial and deep groups of forearm flexor muscles (Figure 2.20) Observe that the median nerve innervates the palmaris longus, flexor carpi radialis, flexor digitorum superficialis, and pronator teres muscles.
- Find the ulnar artery in the cubital fossa. The ulnar artery passes posterior to the deep part of the pronator teres muscle. To follow the ulnar artery distally, release it from the pronator teres muscle by inserting a probe through the pronator teres muscle along the anterior surface of the ulnar artery (posterior to the deep part of the pronator teres muscle). Use scissors to cut the deep part of the pronator teres muscle. The pronator teres muscle is now completely transected and it may be reflected to broaden the dissection field.
- Use a probe to clean the ulnar artery and follow it from the cubital fossa to the wrist. The ulnar vein and its tributaries may be removed to clear the dissection field. Observe that the median nerve crosses anterior to the ulnar artery in the cubital fossa. Note that the ulnar artery passes between the flexor digitorum superficialis and the flexor digitorum profundus muscles (see below) to reach the ulnar (medial) side of the forearm.
- Find the common interosseous artery . It arises about 3 cm distal to the origin of the ulnar artery from the
brachial artery. The common interosseous artery is usually quite short. It passes posterolaterally toward the interosseous membrane
before dividing into the anterior interosseous artery and the posterior interosseous artery.
- Identify the anterior interosseous artery on the anterior surface of the interosseous membrane. The anterior interosseous artery supplies the deep group of flexor muscles.
- The posterior interosseous artery passes posteriorly over the proximal end of the interosseous membrane to reach the posterior compartment of the forearm. The posterior interosseous artery supplies the extensor group of forearm muscles. Identify it, but do not attempt to follow it into the posterior compartment at this time.
- The anterior interossous artery is accompanied by the anterior interosseous nerve. Identify the anterior interosseous nerve, which arises from the median nerve just distal to the cubital fossa and courses distally along the interosseous membrane. The anterior interosseous nerve supplies the radial half of the flexor digitorum profundus and the pronator quadratus.
- Two other named vessels arise from the ulnar artery in the proximal forearm: anterior ulnar recurrent artery and posterior ulnar recurrent artery. They anastomose with the inferior and superior ulnar collateral branches of the brachial artery, respectively (Figure 2.17) Do not attempt to find these vessels. Note that unnamed muscular branches arise from the ulnar artery in the forearm.
- Observe that the ulnar artery joins the ulnar nerve about one-third of the way down the forearm.
- Follow the ulnar nerve proximally and observe that it passes between the two heads of the flexor carpi ulnaris muscle. The ulnar nerve innervates the flexor carpi ulnaris muscle and the medial one-half of the flexor digitorum profundus muscle.
IN THE CLINIC: High Bifurcation of the Brachial Artery
In about 3% of upper limbs, the brachial artery bifurcates in the arm. When it does, the ulnar artery may course superficial to the superficial group of flexor muscles. When this happens, the ulnar artery may be mistaken for a vein. When certain drugs are injected into an artery, the capillary bed is damaged, followed by gangrene. In the example of an injection into a superficial ulnar artery, the hand could be s everely injured.
In about 3% of upper limbs, the brachial artery bifurcates in the arm. When it does, the ulnar artery may course superficial to the superficial group of flexor muscles. When this happens, the ulnar artery may be mistaken for a vein. When certain drugs are injected into an artery, the capillary bed is damaged, followed by gangrene. In the example of an injection into a superficial ulnar artery, the hand could be s everely injured.
Dissection Instructions: Deep Muscles of the Anterior Forearm
- Refer to Figure above but do not cut the flexor pollicis longus muscle as shown in the figure. Three muscles compose the deep group of flexor muscles: flexor digitorum profundus, flexor pollicis longus, and pronator quadratus.
- The proximal attachment of the flexor digitorum profundus muscle is the anterior surface of the ulna and interosseous membrane. Its four tendons lie deep to the four tendons of the flexor digitorum superficialis muscle. Distally, the flexor digitorum profundus tendons attach to the distal phalanges of digits 2 to 5. The flexor digitorum profundus muscle flexes the distal phalanges of digits 2 to 5. The lateral one-half of the flexor digitorum profundus muscle is innervated by the median nerve. The medial one-half of the flexor digitorum profundus muscle is innervated by the ulnar nerve.
- The proximal attachment of the flexor pollicis longus muscle is the anterior surface of the radius and interosseous membrane. The distal attachment of the flexor pollicis longus tendon is the distal phalanx of digit 1 (thumb). The flexor pollicis longus muscle flexes digit 1.
- The pronator quadratus muscle lies deep to the tendons of the superficial and deep flexor muscles. The fibers of the pronator quadratus muscle run transversely from the ulna to the radius in the distal one-fourth of the forearm. Retract the tendons of the superficial and deep groups of flexor muscles and find the pronator quadratus muscle. The pronator quadratus muscle pronates the hand.
- Observe that the anterior interosseous artery and nerve pass deep to the pronator quadratus muscle.
Dissection Review
- Replace the flexor muscles in their correct anatomical positions.
- Use the dissected specimen to review the proximal attachment, distal attachment, and action of each muscle dissected.
- Organize the flexor muscles into a superficial group and a deep group and recall that the nerves and vessels that course through the forearm are found between the two groups.
- Follow the brachial artery from its origin in the proximal arm to its bifurcation in the cubital fossa.
- Review all of the branches of the radial and ulnar arteries. Trace the course of these two arteries from the elbow to the wrist.
- Review the course of the median nerve from the brachial plexus to the wrist.
- Review the course of the ulnar nerve from the brachial plexus to the wrist.
- Recall the rule for innervation of the muscles in the anterior compartment of the forearm:
- All muscles of the anterior compartment of the forearm are innervated by the median nerve except the flexor carpi ulnaris muscle and the medial one-half of the flexor digitorum profundus muscle, which are innervated by the ulnar nerve, and the brachioradialis muscle, which is supplied by the radial nerve.
DISSECTION LABORATORY #3: PALMAR HAND
By definition, intrinsic hand muscles are muscles that have their proximal and distal attachments within the hand. There are two superficial groups of intrinsic hand muscles: The thenar group of muscles forms the thenar eminence, and the hypothenar group of muscles forms the hypothenar eminence. Deep in the hand is a third group of intrinsic hand muscles: the interosseous muscles and the adductor pollicis muscle.
In the middle of the palm, the palmar fascia is thickened to form the palmar aponeurosis. The palmar fascia over the thenar and hypothenar eminences is much thinner. Deep to the palmar aponeurosis are the tendons of the flexor digitorum superficialis and flexor digitorum profundus muscles. These tendons reach the palm through the carpal tunnel and are responsible for flexing the digits. In the deepest part of the palm are muscles that abduct and adduct the digits.
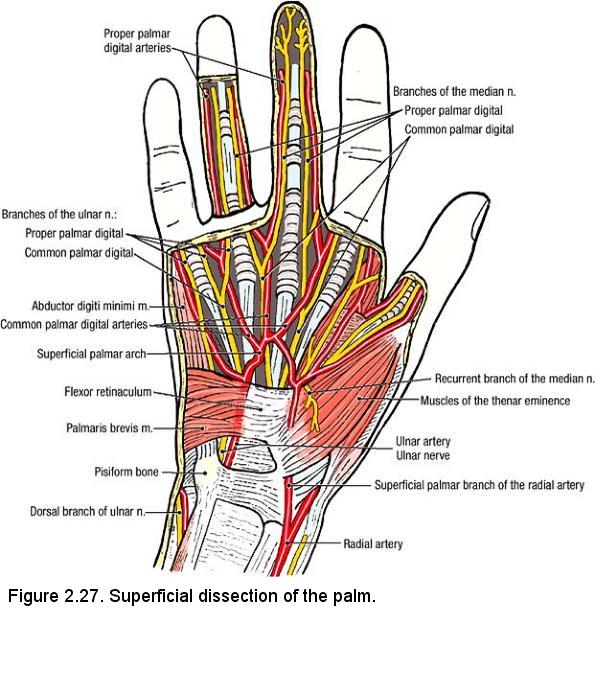
The palm is supplied with blood by two arterial arches. The superficial palmar arch is mainly derived from the ulnar artery and the deep palmar arch from the radial artery. The nerve supply of the palmar aspect of the hand is derived from the median and ulnar nerves.
The order of dissection will be as follows: The palmar aponeurosis will be studied and removed. The superficial palmar arch will be dissected, followed by the tendons of the muscles of the anterior compartment of the forearm. The flexor retinaculum will be cut and the flexor tendons will be released from the palm. The muscles of the thenar group will be dissected, followed by the muscles of the hypothenar group. The deep palmar arch will be dissected along with the deep branch of the ulnar nerve. The interosseous muscles will be studied.
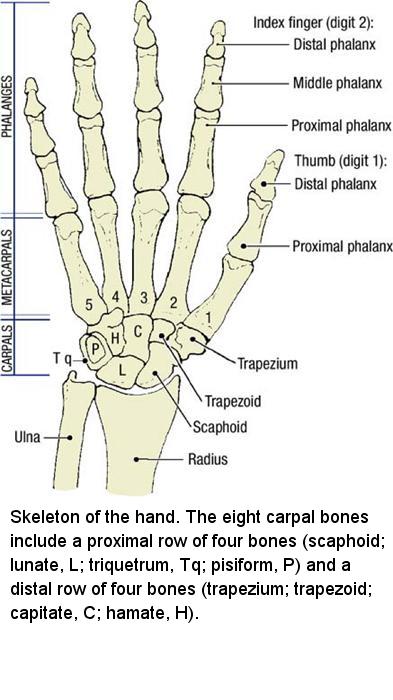
Osteology
Refer to an articulated skeleton of the hand and identify:
- Eight carpal bones (Gr. karpos, wrist): scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, hamate
- Five metacarpal bones and their base, shaft, and head
- 14 phalanges
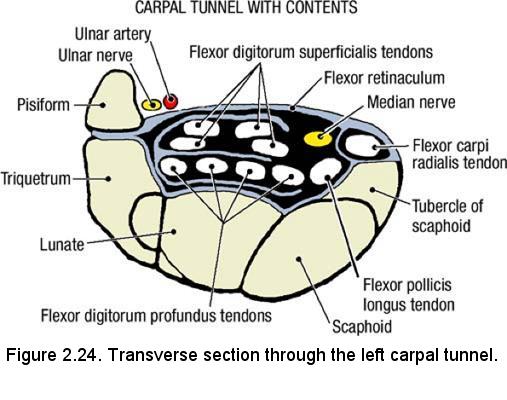
pisiform bone and the hook of the hamate on the medial side of the wrist. On the lateral side of the wrist, identify the tubercle of the scaphoid and the tubercle of the trapezium. The flexor retinaculum bridges these four bones (Figure 2.24). The space between the carpal bones and the flexor retinaculum is the carpal tunnel, which allows passage of the flexor tendons and the median nerve into the hand.
Dissection Instructions: Superficial Palm
Skin Incisions:
- Force open the clenched hand and use a bungee cord to tie the open fingers to the board. When working with the bungee cords, be sure that they are securely fastened and take extra care when unfastening these cords. They are under tension and the metal hooks may fly freely with high velocity.
- Make a longitudinal incision across the middle of the palm.
- Make a longitudinal incision on the anterior surface of the middle digit.
- Remove the skin from the palmar surface of the hand and the middle digit. When skinning the digit, proceed with caution. Note that the subcutaneous tissue on the palmar surface of the digits is very thin, especially at the skin creases. There are digital nerves, vessels, and fibrous digital sheaths immediately deep to the skin.
- Use scraping motions with a dull scalpel blade to clean the fat from the palmar aponeurosis. Observe that the palmar aponeurosis has four bands of longitudinal fibers, one band to each of digits 2 to 5. These longitudinal fibers end by attaching to the fibrous digital sheath near the base of the proximal phalanx of each digit.
- Identify the palmar fascia covering the thenar muscles lateral to the palmar aponeurosis.
- Identify the palmar fascia covering the hypothenar muscles medial to the palmar aponeurosis. The palmaris brevis muscle is found superficial to the hypothenar muscles (Figure 2.27). It is a thin, fragile muscle. The proximal attachment of the palmaris brevis muscle is the medial aspect of the palmar aponeurosis. Its distal attachment is the skin over the hypothenar eminence.
- Detach the palmaris brevis muscle from the palmar aponeurosis and reflect it medially (You may have already accidently removed this muscle. Don't worry. It's okay!).
- Find the tendon of the palmaris longus muscle where you transected it in the forearm. Follow the palmaris longus tendon distally into the palm where it is attached to the palmar aponeurosis. Although the palmaris longus muscle may be absent, the palmar aponeurosis is always present.
- To remove the palmar aponeurosis, use a scalpel and skinning motions to detach the palmar aponeurosis from the underlying deep structures.
Begin at its proximal end and proceed distally. Use the palmaris longus tendon to apply traction to the palmar aponeurosis during its
removal. Do not cut too deeply, as the superficial palmar arch is in contact with the deep surface of the palmar aponeurosis.
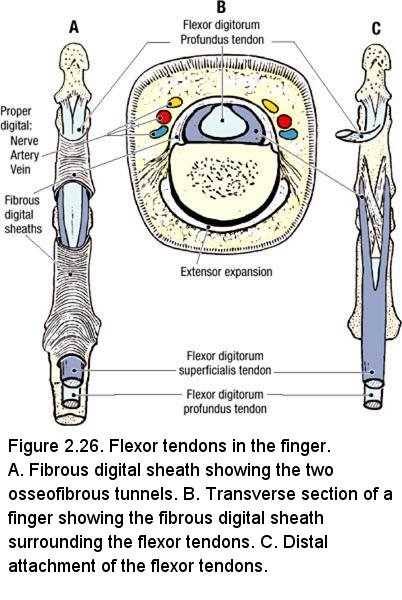
- Near the proximal end of digit 3, remove each band of longitudinal fibers of the palmar aponeurosis. Use blunt dissection to clean the fibrous digital sheath on the flexor surface of the digit (Figure 2.26).
- Find the ulnar artery in the forearm. Use a probe to dissect the ulnar artery and follow it into the palm. The ulnar artery passes lateral to the pisiform bone with the ulnar nerve, then divides into two branches: the superficial palmar arch and the deep palmar branch of the ulnar artery. The superficial palmar arch is completed by a smaller contribution from the superficial palmar branch of the radial artery (Figure 2.27).
- Use a probe to clean the superficial palmar arch and the three common palmar digital arteries arising from it. Trace one common palmar digital artery distally and note that it divides into two proper palmar digital arteries that supply the opposing sides of two adjacent digits.
- Find the ulnar nerve lateral to the pisiform bone. Use a probe to dissect the superficial branch of the ulnar nerve, which supplies cutaneous innervation to digit 5 and the medial side of digit 4. The deep branch of the ulnar nerve accompanies the deep palmar branch of the ulnar artery and disappears into the hypothenar muscles. Identify the initial portion of the deep branch of the ulnar nerve but do not follow it at this time.
Dissection Instructions: Carpal Tunnel
- Identify the flexor retinaculum between the thenar and hypothenar eminences (Figure 2.27). Use an illustration to review the flexor retinaculum and its role in the formation of the carpal tunnel (Figure 2.24).
- Insert a probe from proximal to distal, deep to the flexor retinaculum (Figure 2.28). Push the probe as far medial as possible to protect
the median nerve and the recurrent branch of the median nerve. Use a scalpel to cut through the flexor retinaculum to the probe. Open
the carpal tunnel.
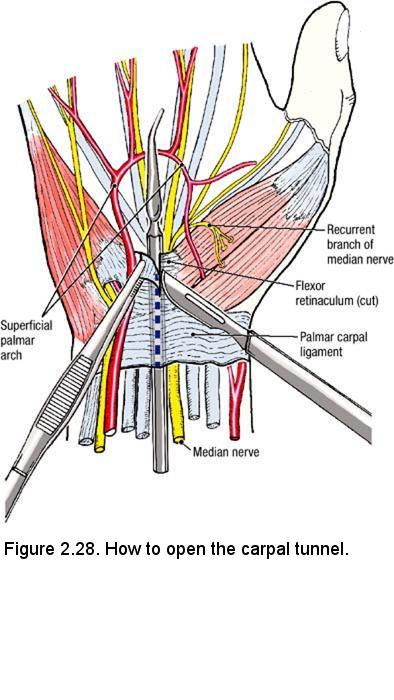
- Examine the contents of the carpal tunnel: median nerve, four tendons of the flexor digitorum superficialis muscle, four tendons of the flexor digitorum profundus muscle, and the tendon of the flexor pollicis longus muscle (Figure 2.24).
- Find the median nerve at the level of the wrist and follow it through the carpal tunnel. Identify the recurrent branch of the median nerve, which innervates the three thenar muscles (Figure 2.28). The median nerve also innervates lumbrical muscles 1 and 2.
- From the median nerve follow common palmar digital nerves into the lateral 3½ digits (Figure 2.27). Note that the common palmar digital nerves typically divide to give rise to two proper palmar digital nerves, which accompany the proper palmar digital arteries. Use an illustration to study the cutaneous distribution of the median nerve in the hand.
- Identify the flexor tendons that pass through the carpal tunnel. Observe that these tendons pass through the palm of the hand posterior to the superficial palmar arch and digital nerves. The flexor tendons enter the fibrous digital sheaths on the anterior surfaces of the digits (Figure 2.26).
- Use an illustration to study the extent of the synovial tendon sheaths deep to the flexor retinaculum and extending into the palm. There are two sets of synovial sheaths: one common flexor synovial sheath (ulnar bursa) and three digital synovial sheaths. The tendon of the flexor pollicis longus muscle has it own synovial sheath (radial bursa).
IN THE CLINIC: Dupuytren's Contracture
Idiopathic shortening and thickening of the longitudinal bands of the palmar aponeurosis, especially in middle aged men, can lead to traction and radial deviation of the medial digits.
Idiopathic shortening and thickening of the longitudinal bands of the palmar aponeurosis, especially in middle aged men, can lead to traction and radial deviation of the medial digits.
IN THE CLINIC: Carpal Tunnel Syndrome
A swelling of the common flexor synovial sheath may encroach on the available space in the carpal tunnel. As a result, the median nerve may be compressed, resulting in pain and paresthesia of the thumb and index and middle fingers, and weakness of the thenar muscles.
A swelling of the common flexor synovial sheath may encroach on the available space in the carpal tunnel. As a result, the median nerve may be compressed, resulting in pain and paresthesia of the thumb and index and middle fingers, and weakness of the thenar muscles.
Dissection Instructions: Thenar Compartment
- Prior to dissecting, study an illustration of the thenar group of muscles (Figure 2.27). The thenar group contains three muscles:
abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis (L. pollex, thumb; genitive,
pollicis, meaning "of the thumb"). The proximal attachments of the thenar muscles are the lateral carpal bones.
- Abductor pollicis brevis muscle inserts into the lateral side of the proximal phalanx of the thumb and abducts the thumb.
- Flexor pollicis brevis muscle inserts into the lateral side of the proximal phalanx of the thumb and flexes the thumb.
- Opponens pollicis muscle attaches to the lateral side of the first metacarpal bone and opposes the thumb.
- Trace the median nerve to find the recurrent branch of the median nerve (Figure 2.28). The recurrent branch of the median nerve crosses the superficial surface of the flexor pollicis brevis muscle, then disappears deep to the abductor pollicis brevis muscle.
- Use blunt dissection to clean the palmar fascia off the thenar muscles. Preserve the recurrent branch of the median nerve.
- Use a probe to separate the abductor pollicis brevis muscle from the flexor pollicis brevis muscle. Use the recurrent branch of the median nerve to help you locate the correct plane of separation.
- Use a probe to elevate the abductor pollicis brevis muscle and transect it with scissors.
- Observe the opponens pollicis muscle deep to the abductor pollicis brevis muscle. Note that the opponens pollicis muscle attaches to the entire length of the lateral side of the first metacarpal bone.
IN THE CLINIC: Recurrent Branch of the Median Nerve
The recurrent branch of the median nerve is superficial and it can easily be severed by "minor" cuts over the thenar eminence. If the recurrent branch of the median nerve is injured, the thenar muscles are paralyzed and the thumb cannot be opposed.
The recurrent branch of the median nerve is superficial and it can easily be severed by "minor" cuts over the thenar eminence. If the recurrent branch of the median nerve is injured, the thenar muscles are paralyzed and the thumb cannot be opposed.
Dissection Instructions: Hypothenar Compartment
- Use blunt dissection to clean the palmar fascia off the hypothenar muscles (Figure 2.28). The hypothenar group contains three muscles:
abductor digiti minimi, flexor digiti minimi (brevis), and opponens digiti minimi. The proximal attachments of the
hypothenar muscles are the medial carpal bones.
- Abductor digiti minimi muscle insert into the medial side of the proximal phalanx of digit 5 and abducts digit 5.
- Flexor digiti minimi (brevis) muscle inserts into the medial side of the proximal phalanx of digit 5 and flexes digit 5.
- Opponens digiti minimi muscle attaches to the medial border of the fifth metacarpal bone and opposes digit 5.
- Find the tendons of the abductor digiti minimi and flexor digiti minimi (brevis) muscles near their distal attachments to the medial side of the base of the proximal phalanx. Use a probe to separate and define the borders of the muscles using their tendons to aid in this separation.
- Use a probe to elevate the abductor digiti minimi muscle and detach it from its proximal attachment on the flexor retinaculum. Preserve the deep branches of the ulnar artery and ulnar nerve. Reflect the muscle distally.
- Observe the opponens digiti minimi muscle. Note that the opponens digiti minimi muscle attaches to the entire length of the fifth metacarpal bone.
Dissection Instructions: Deep Palm (TO BE CARRIED OUT ON ONE SIDE ONLY)
- At this time examine your cadaver's palm and the palm that your partner dissected. Decide which is better. If you have difficulty, call over an instructor to make the decision. Since the dissection of the deep palm will destroy the superficial structures, the side with the better superficial dissection should be preserved. Do the deep dissection on the other side.
- In the distal forearm, use your fingers to separate the tendons of the flexor digitorum superficialis muscle from the tendons of the flexor digitorum profundus muscle. About 5 cm proximal to the wrist, use scissors to transect the tendons of the flexor digitorum superficialis muscle. Reflect the tendons distally, pulling them through the carpal tunnel. During this procedure, the common flexor synovial sheath (ulnar bursa) will be destroyed. To reflect the tendons even further, cut the superficial palmar arch in the midline of the palm, retract the common digital branches of the median and ulnar nerves, and make a longitudinal slit in the fibrous digital sheaths of digit 3.
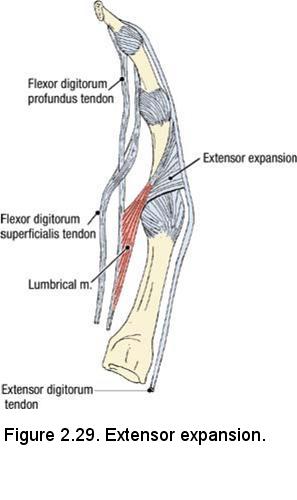
- In the palm, observe the tendons of the flexor digitorum profundus muscle. Identify four lumbrical muscles that are attached to the four tendons of the flexor digitorum profundus muscle. The distal attachment of the lumbrical muscles is the radial side of the extensor expansions of digits 2 to 5 (Figure 2.29). The lumbrical muscles flex the metacarpophalangeal joints and extend the interphalangeal joints.
- In digit 3, study the relationship of the tendons of the flexor digitorum superficialis and flexor digitorum profundus muscles (Figure 2.29). Note that the flexor digitorum profundus tendon passes through the flexor digitorum superficialis tendon. Verify that the flexor digitorum superficialis tendon attaches to the middle phalanx, whereas the flexor digitorum profundus tendon attaches to the distal phalanx. This pattern is true of digits 2 to 5.
- Identify the flexor pollicis longus muscle in the forearm. Follow its tendon distally through the carpal tunnel into the palm. Pull on the tendon to confirm that the flexor pollicis longus muscle attaches to the distal phalanx of the thumb.
- Transect the flexor digitorum profundus muscle in the distal one-third of the forearm. Reflect its tendons and the associated lumbrical muscles distally as far as possible. The deep palm is now exposed.
- Find the ulnar nerve and the ulnar artery on the lateral side of the pisiform bone.
- The deep branch of the ulnar nerve and the deep palmar branch of the ulnar artery pass between the proximal attachments of the flexor digiti minimi (brevis) and abductor digiti minimi muscles.
- Push a probe parallel to the deep branch of the ulnar nerve where it pierces the opponens digiti minimi muscle. Use a scalpel to cut down
to the probe. Use blunt dissection to follow the deep branch of the ulnar nerve into the palm.
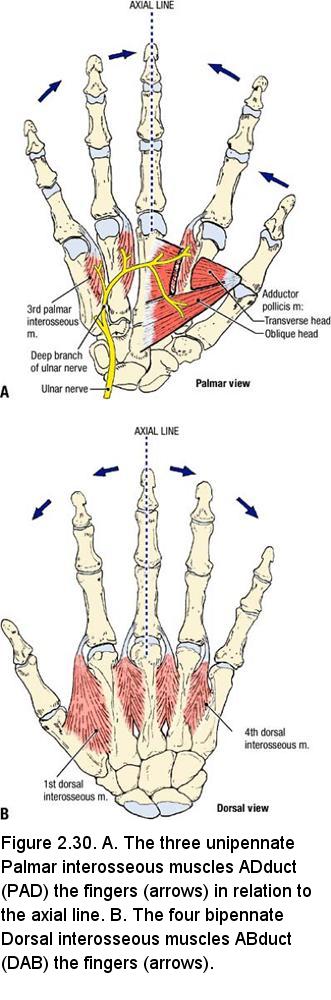
- Observe that the deep branch of the ulnar nerve lies on the anterior surface of the interosseous muscles (Figure 2.30A).
- Observe the deep palmar arch. The deep palmar arch courses with the deep branch of the ulnar nerve. The deep palmar arch arises from the radial artery. The deep palmar arch is completed by the deep branch of the ulnar artery. Use an illustration to study the branches of the deep palmar arch.
- Observe that the deep palmar arch crosses the palm proximal to the superficial palmar arch.
- Identify the adductor pollicis muscle (Figure 2.30A). Use blunt dissection to define its borders. The adductor pollicis muscle has two heads: oblique and transverse. The proximal attachments of the oblique head are the bases of metacarpal bones 2 and 3 and the adjacent carpal bones. The proximal attachment of the transverse head is the anterior surface of the shaft of metacarpal bone 3. Both heads attach to the medial side of the base of the proximal phalanx of the thumb. The adductor pollicis muscle draws the thumb toward digit 3 (adduction).
- Identify the three palmar interosseous muscles (Figure 2.30A). The palmar interosseous muscles are unipennate muscles that attach to the metacarpal bones of digits 2, 4, and 5. Distally, each palmar interosseous muscle attaches to the base of the proximal phalanx and the extensor expansion of the same digit on which it originates.
- Use an illustration to study the four dorsal interosseous muscles (Figure 2.30B). The dorsal interosseous muscles are bipennate muscles that attach to metacarpal bones 1 to 5. Distally, the dorsal interosseous muscles attach to the bases of the proximal phalanges and the extensor expansions of digits 2 to 4. Look at the dorsum of the dissected hand and note that the dorsal interosseous muscles occupy the intervals between the metacarpal bones. Identify only the first dorsal interosseous muscle. The first dorsal interosseous muscle may atrophy following an injury to the ulnar nerve.
- Study the actions of the interosseous muscles (Figure 2.30A,B). The three Palmar interosseous muscles are ADductors (PAD). They adduct digits 2, 4, and 5 toward an imaginary axial line drawn through the long axis of digit 3. The four Dorsal interosseous muscles are ABductors (DAB). They move digits 2 to 4 away from the imaginary axial line. The two dorsal interosseous muscles that attach to digit 3 move it to either side of the imaginary axial line. The interosseous muscles are innervated by the deep branch of the ulnar nerve.
Dissection Review
- Place the muscles, tendons, and nerves that you have dissected back into their correct anatomical positions.
- Review the movements of the fingers and thumb. Define flexion, extension, abduction, and adduction. Review the muscles that are responsible for each action.
- Use the dissected specimen to follow the median nerve from the forearm into the hand. Review its recurrent branch and list the three muscles that the recurrent branch innervates.
- Follow the ulnar artery from the elbow to the hand. In the hand, trace the superficial branch and deep palmar branch of the ulnar artery.
- Follow the ulnar nerve from the medial epicondyle of the humerus to the hand. In the hand, trace the superficial and deep branches of the ulnar nerve.
- Review an illustration that demonstrates the cutaneous distribution of the ulnar and median nerves in the hand.
- Recall the rule for innervation of the muscles in the hand:
- All intrinsic muscles of the hand are innervated by the ulnar nerve except the muscles of the thenar group and the first two lumbrical muscles, which are innervated by the median nerve.
DISSECTION LABORATORY #4: THE SCAPULAR REGION, POSTERIOR COMPARTMENTS OF THE ARM AND FOREARM
Upon completion of this session, the student will be able to:
- Identify the posterior shoulder muscles and associated rotator cuff muscles. Give their general functions and nerve supply.
- Identify and demonstrate the regional blood supply of the posterior shoulder.
- Describe the functional deficits associated with injury to the superficial back muscles and the muscles of the scapular region
- Identify prominent features of the humerus, ulna, radius, carpals, metacarpals and phalanges as given in the lab manual.
- Identify the contents of posterior compartment of the arm and the functional significance of the included muscles.
- Correlate any fractures of the humerus with functional disruptions of associated muscular and neurovascular structures.
- Identify spatial relationships of all associated muscular and neurovascular structures within the posterior arm.
- Identify the extensor compartment of the forearm and hand, the nerve and vessels supplying their contents, and the functional significance of the included muscles.
- Correlate any fractures or deep cuts of the forearm or hand with functional disruptions of associated muscular or neurovascular structures.
- Identify position of tendons and associated bursae beneath the extensor retinaculum.
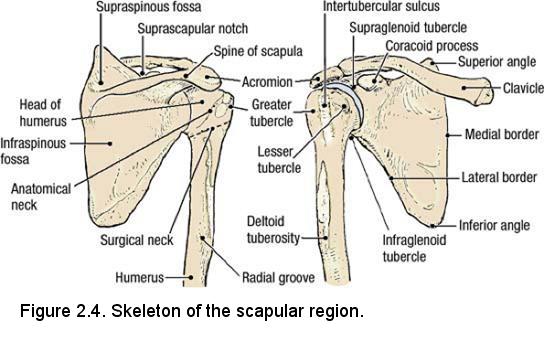
Osteology of the Scapular Region
Refer to a skeleton. On the scapula, identify (Figure 2.4):
- Acromion
- Suprascapular notch
- Supraspinous fossa
- Spine
- Infraspinous fossa
- Supraglenoid tubercle
- Glenoid cavity
- Infraglenoid tubercle
- Coracoid process
- Head
- Anatomical neck
- Greater tubercle
- Lesser tubercle
- Intertubercular sulcus (bicipital groove)
- Surgical neck
- Deltoid tuberosity
- Radial groove
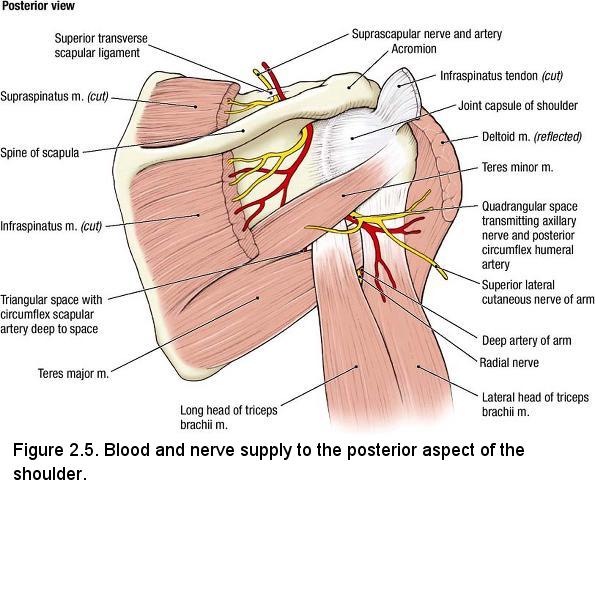
Dissection Overview: Scapular Region
There are six shoulder (scapulohumeral) muscles: deltoid, supraspinatus, infraspinatus, teres minor, teres major, and subscapularis. The order
of dissection will be as follows: The deltoid muscle will be studied, and then it will be detached from its proximal attachment and the
course of its nerve and artery will be studied. Subsequently, the four muscles arising from the dorsal surface of the scapula (supraspinatus,
infraspinatus, teres major, teres minor) will be dissected and their nerves and blood vessels will be demonstrated. The subscapularis muscle
was dissected with the axilla.
Dissection Instructions: Scapular Region
- Place the cadaver in the prone position (face down). Abduct the upper limb to 45°. If a block is available, place it under the chest.
- Remove any remaining skin from the upper limb. Do so gently on the dorsum of the hand, taking care to preserve underlying structures.
- Use blunt dissection to define the borders of the deltoid muscle. The proximal attachments of the deltoid muscle are the spine and acromion of the scapula, and the lateral one-third of the clavicle. The distal attachment of the deltoid muscle is the deltoid tuberosity of the humerus. The deltoid muscle flexes, abducts, and extends the humerus.
- Use a scalpel to detach the deltoid muscle from the spine of the scapula and acromion leaving it attached to the clavicle. Make your cuts close to the bone. Reflect the deltoid muscle anteriorly, taking care not to tear the vessels and nerve that course along its deep surface.
- Observe the axillary nerve and the posterior circumflex humeral artery and vein on the deep surface of the deltoid muscle near its attachment to the humerus. Use a probe to clean the nerve and vessels and trace them around the surgical neck of the humerus (Figure 2.5). Note that the axillary nerve innervates the deltoid muscle and the teres minor muscle.
- Follow the axillary nerve and the posterior circumflex humeral artery and vein deeply. Push your finger parallel to the nerve and vessels
to open the quadrangular space (Figure 2.5). Define the borders of the quadrangular space:
- Superior border - inferior border of the teres minor muscle
- Lateral border - surgical neck of the humerus
- Medial border - long head of the triceps brachii muscle
- Inferior border - superior border of the teres major muscle
- Identify the long head of the triceps brachii muscle. Observe that the long head of the triceps brachii muscle passes anterior to the teres minor muscle and posterior to the teres major muscle.
- Use a probe to clean and define the borders of the teres minor muscle. The proximal attachment of the teres minor muscle is the lateral border of the scapula. The distal attachment of the teres minor muscle is the greater tubercle of the humerus. The teres minor muscle laterally rotates the humerus.
- Clean and define the borders of the teres major muscle. The proximal attachment of the teres major muscle is the inferior angle of the scapula. The distal attachment of the teres major muscle is the intertubercular sulcus of the humerus. The teres major muscle adducts and medially rotates the humerus.
- Define the borders of the triangular space:
- Superior border - inferior border of the teres minor muscle
- Lateral border - tendon of the long head of the triceps brachii muscle
- Inferior border - superior border of the teres major muscle
- Note that the circumflex scapular artery may be found deep within the triangular space.
- Reflect the trapezius muscle superiorly, leaving it attached along the "hinge" of cervical fascia that was created during the back dissection.
- Clean and define the borders of the supraspinatus muscle. The proximal attachment of the supraspinatus muscle is the supraspinous fossa of the scapula. The distal attachment of the supraspinatus muscle is high up on the greater tubercle of the humerus. The supraspinatus muscle initiates abduction of the humerus.
- Use a probe to define the borders of the infraspinatus muscle. The proximal attachment of the infraspinatus muscle is the infraspinous fossa of the scapula. The distal attachment of the infraspinatus muscle is the greater tubercle of the humerus. The infraspinatus muscle laterally rotates the humerus.
- The suprascapular artery and the suprascapular nerve are found deep to the supraspinatus muscle (Figure 2.5). To see them, the supraspinatus muscle must be reflected. Use a scalpel to transect the supraspinatus muscle about 5 cm lateral to the superior angle of the scapula but medial to the suprascapular notch. Hold a disarticulated scapula over the scapula of the cadaver to help you locate the proper level of the cut.
- Use blunt dissection to loosen, from the supraspinous fossa, the portion of the supraspinatus muscle that is distal to the transection. Reflect it laterally. Leave it attached to the humerus.
- Identify the suprascapular artery and nerve. Follow the artery and nerve superiorly. Observe that the suprascapular artery passes superior to the superior transverse scapular ligament and the suprascapular nerve passes inferior to it (Figure 2.5). This relationship can be remembered by use of a mnemonic device: "Army (artery) goes over the bridge; Navy (nerve) goes under the bridge."
- Transect the infraspinatus muscle about 5 cm lateral to the vertebral border of the scapula (Figure 2.5).
- Use blunt dissection to loosen, from the infraspinous fossa, the portion of the infraspinatus muscle that is distal to the transection. Reflect it laterally.
- Follow the suprascapular artery and the suprascapular nerve inferiorly. Note that they reach the infraspinatus muscle by coursing deep (anterior) to the spine of the scapula (Figure 2.5).
- The suprascapular artery contributes to the collateral circulation of the scapular region. Use an illustration to study the scapular anastomosis.
- The four muscles of the rotator cuff are the supraspinatus, infraspinatus, teres minor, and the subscapularis. Use an illustration to study the distal attachments of the rotator cuff muscles.
Dissection Review
- Replace the muscles of the scapular region in their correct anatomical positions.
- Use an illustration and the dissected specimen to review the proximal attachment and distal attachment of each muscle of the scapular region. List the action of each muscle and the combined action of the rotator cuff group of muscles.
- Review the origin, course, and distribution of the transverse cervical artery, dorsal scapular artery, and suprascapular artery.
- Review the scapular anastomosis.
- Review the relationship of the suprascapular artery and the suprascapular nerve to the superior transverse scapular ligament.
- Review the innervation of each muscle dissected today.
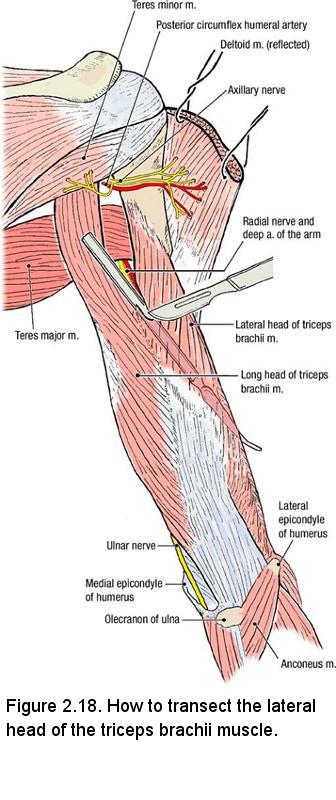
Dissection Instructions: Posterior Compartment of the Arm
- Place the cadaver in the prone position.
- To gain better access to the posterior compartment, rotate the arm medially.
- Use scissors to open the posterior compartment of the arm by making a longitudinal incision through the brachial fascia from the level of the olecranon of the ulna to the teres minor muscle.
- Use your fingers to clean and define the borders of the triceps brachii muscle. The triceps brachii muscle has three proximal
attachments:
- Long head of the triceps brachii muscle attaches to the infraglenoid tubercle of the scapula.
- Lateral head of the triceps brachii muscle attaches to the posterior surface of the humerus superior to the radial groove.
- Medial head of the triceps brachii muscle attaches to the posterior surface of the humerus inferior to the radial groove.
- Observe the distal attachment of the triceps brachii tendon on the olecranon of the ulna. The triceps brachii muscle extends the forearm.
- Use your fingers to separate the long head of the triceps brachii from the lateral head. Observe that the teres major muscle crosses the anterior surface of the long head.
- Inferior to the teres major muscle is an opening between the long head of the triceps brachii muscle and lateral head of the triceps brachii muscle (Figure 2.18). Use a probe to widen this opening and identify the radial nerve and the deep artery of the arm.
- Push a probe distally along the course of the radial nerve. The probe should be positioned between the lateral head of the triceps brachii muscle and the humerus (Figure 2.18).
- Use a scalpel to transect the lateral head of the triceps brachii muscle over the probe. This cut will separate the lateral head of the triceps brachii muscle from the medial head.
- Use a probe to clean the radial nerve and the deep artery of the arm. Observe that the radial nerve and deep artery of the arm lie directly on the posterior surface of the humerus in the radial groove.
- Confirm the course of the radial nerve through the posterior compartment to the elbow. To do this, return to the cubital fossa. On the lateral aspect of the forearm, identify the brachioradialis muscle. Use your fingers to open the connective tissue plane between the brachioradialis muscle and the brachialis muscle. Deep in this plane of connective tissue, find the radial nerve and follow it proximally.
- Note that the radial nerve passes on the flexor side of the elbow joint and that it is accompanied by the radial recurrent artery at that location (Figure 2.16).
- Identify the anconeus muscle (Figure 2.18). The proximal attachment of the anconeus muscle is the lateral epicondyle of the humerus. The distal attachment is the lateral surface of the olecranon and superior part of the posterior surface of the ulna. The anconeus muscle assists the triceps brachii muscle in extension of the forearm.
Dissection Review
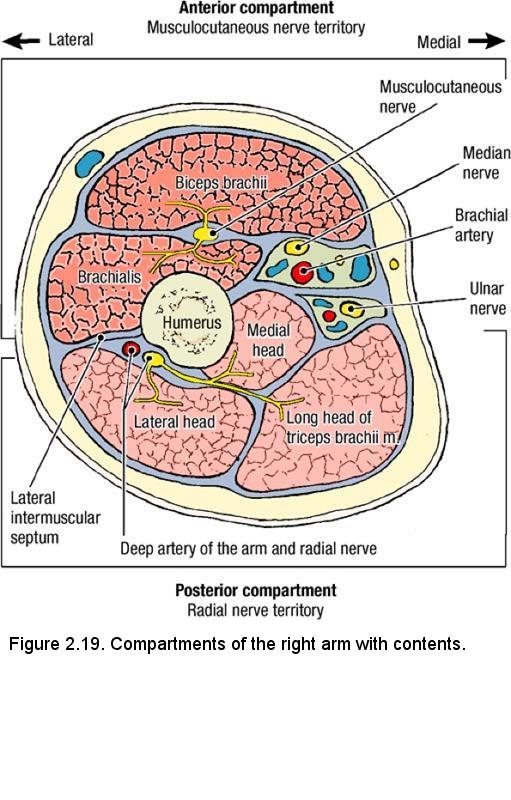
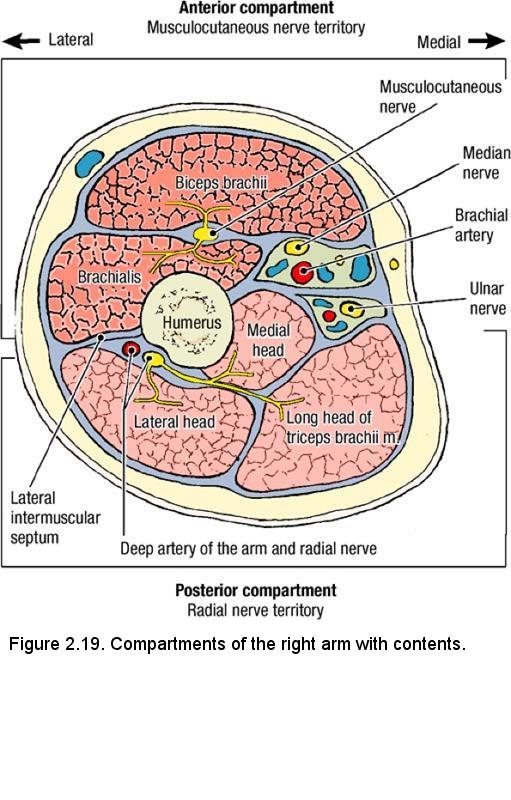
- Replace the muscles of the anterior compartment of the arm in their correct anatomical positions.
- Review the proximal attachment, distal attachment, nerve, and action of each muscle.
- Use the dissected specimen to review the origin, course, termination, and branches of the brachial artery.
- Trace each nerve that you have dissected from the brachial plexus to the elbow, reviewing relationships.
- Review a drawing of a cross section of the arm and notice the position of the brachial fascia and the intermuscular septa relative to the structures that you have dissected.
- Review the nerve territories of the brachial region (Figure 2.19).
- Recall the rules of innervation of the muscles of the arm:
- All muscles in the anterior compartment of the arm are innervated by the musculocutaneous nerve
- All muscles in the posterior compartment of the arm are innervated by the radial nerve.
- The median nerve and the ulnar nerve do not innervate muscles in the arm.
Dissection Overview: Posterior Compartment of the Forearm
The posterior compartment of the forearm contains the extensor muscles of the hand and digits. They can be divided into a superficial group and a
deep group (Figure 2.20). The muscles of the superficial group extend the wrist and the proximal phalanges. The muscles of the deep group of
extensors cause supination of the hand, extension of digit 2, and abduction and extension of the thumb. The deep branch of the radial nerve
innervates the extensor muscles of the forearm. Nerves and vessels of the posterior compartment run in the connective tissue plane that divides the
superficial group of extensor muscles from the deep group of extensor muscles (Figure 2.20).
In the dorsum of the hand, the bones are superficial. There are no intrinsic muscles in the dorsum of the hand, so no motor innervation is required. The radial, ulnar, and median nerves share the cutaneous innervation of the dorsum of the hand.
The order of dissection will be as follows: The antebrachial fascia will be removed from the elbow to the wrist. The muscles of the superficial extensor group will be identified and followed to their distal attachments in the hand. The tendons of the superficial extensor muscles will be released from the extensor retinaculum and retracted to permit the muscles of the deep extensor group to be studied. The contents of the anatomical snuffbox will be identified.
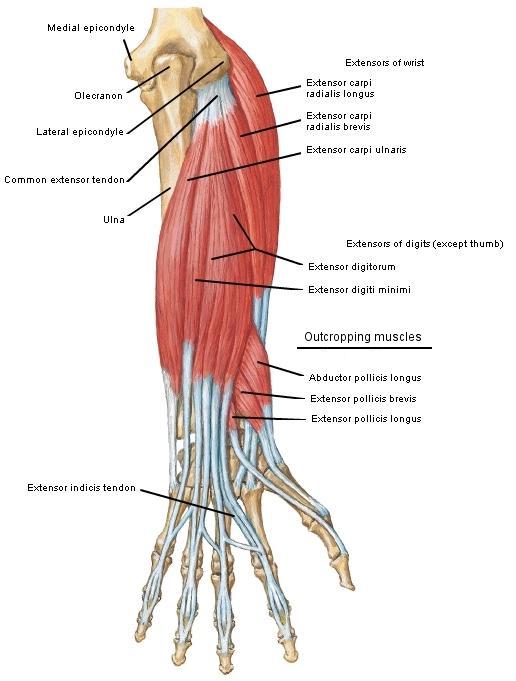
Dissection Instructions: Superficial Muscles of the Posterior Forearm Compartment
- Place the cadaver in the supine position.
- Use blunt dissection to remove the remnants of the superficial fascia from the posterior forearm and dorsum of the hand, taking care to preserve the dorsal venous arch, if possible (but don't grow old doing this).
- Identify the extensor retinaculum, which is a specialization of the antebrachial fascia located on the posterior surface of the distal forearm.
- Use scissors to incise the posterior surface of the antebrachial fascia from the olecranon to the extensor retinaculum. Preserve the extensor retinaculum. Use your fingers or a probe to separate the antebrachial fascia from the muscles that lie deep to it. Detach the antebrachial fascia from its attachments to the radius and ulna and place it in the tissue container.
- Six muscles compose the superficial group: brachioradialis (a forearm flexor that has rotated to the anterolateral aspect of the forearm), extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris. Note that four of the muscles in the superficial group (extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris) attach to the lateral epicondyle of the humerus by way of a common extensor tendon.
- Use tendon patterns at the wrist and distal attachments to positively identify the muscles of the superficial group:
- Brachioradialis tendon attaches to the lateral surface of the distal radius.
- Extensor carpi radialis longus tendon attaches to the base of metacarpal bone 2.
- Extensor carpi radialis brevis tendon attaches to the base of metacarpal bone 3.
- Extensor digitorum tendons attach to the extensor expansions of digits 2 to 5.
- Extensor digiti minimi tendon attaches to the extensor expansion of digit 5.
- Extensor carpi ulnaris tendon attaches to the base of metacarpal bone 5.
- Note that the tendons of the extensor digitorum muscle are tied together by intertendinous connections on the posterior surface of the hand.
- Observe the extensor expansion of digit 3 (Figure 2.29). The extensor expansion is wrapped around the dorsum and the sides of the proximal phalanx and the distal end of the metacarpal bone. The hood-like expansion retains the extensor tendon in the midline of the digit. The tendons of the lumbrical and interosseous muscles attach to the extensor expansion.
- Cut through the extensor retinaculum to release the tendons of the extensor digitorum muscle. Retract the tendons medially. Note that the other extensor tendons are also contained within individual osseofibrous tunnels. Synovial sheaths line these tunnels.
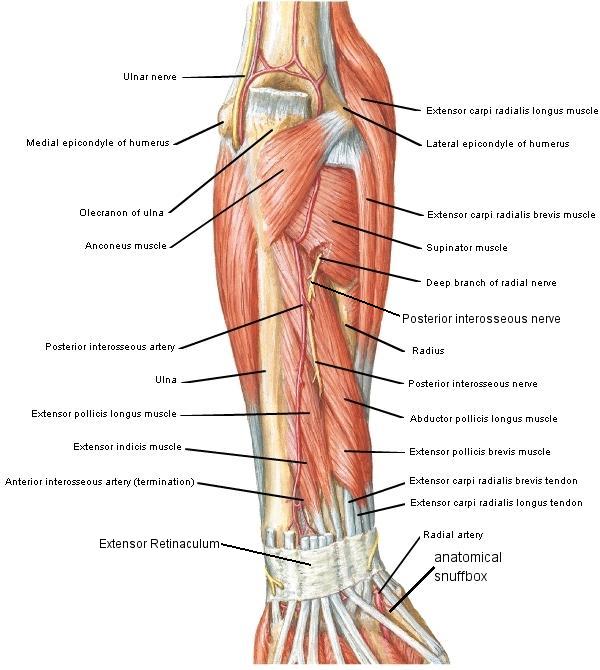
Dissection Instructions: Deep Muscles of the Posterior Forearm Compartment
- Five muscles compose the deep group: abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, extensor indicis, and supinator.
- The proximal attachments of four muscles of the deep group (abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis) are the posterior surfaces of the radius, ulna, and interosseous membrane. These four muscles emerge from the interval between the extensor digitorum muscle and the extensor carpi radialis brevis muscle.
- Observe the tendon of each of the following muscles and follow it to its distal attachment:
- Abductor pollicis longus tendon attaches to the base of metacarpal bone 1.
- Extensor pollicis brevis tendon attaches to the base of the proximal phalanx of digit 1.
- Extensor pollicis longus tendon attaches to the base of the distal phalanx of digit 1.
- Extensor indicis tendon attaches to the extensor expansion of digit 2.
- Identify the anatomical snuffbox (Figure 2.31). The anatomical snuffbox is a depression on the posterior surface of the wrist that is bounded anteriorly by the abductor pollicis longus tendon and the extensor pollicis brevis tendon. The posterior boundary of the anatomical snuffbox is the extensor pollicis longus tendon.
- Within the anatomical snuffbox, find the radial artery. Use a probe to clean the radial artery and follow it distally until it disappears between the two heads of the first dorsal interosseous muscle. Note that the dorsal carpal arch is a branch of the radial artery that arises in the anatomical snuff box. The dorsal carpal arch supplies arterial blood to the dorsum of the hand (Figure 2.31). Do not dissect its branches.
- Near the elbow, use your fingers to retract the brachioradialis muscle and observe the supinator muscle. The proximal attachments
of the supinator muscle are the lateral epicondyle of the humerus, the radial collateral and anular ligaments of the elbow, and the
olecranon of the ulna. The distal attachment of the supinator muscle is the proximal one-third of the radius. The supinator muscle supinates
the hand.
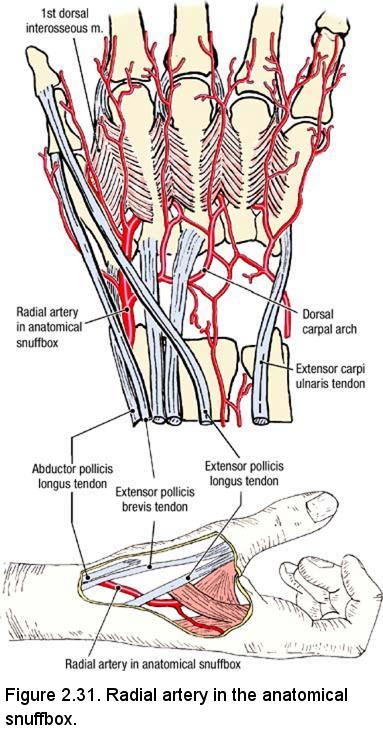
- On the lateral aspect of the elbow, once again find the radial nerve in the connective tissue plane between the brachioradialis muscle and the brachialis muscle. Observe that the radial nerve divides into a superficial branch and a deep branch. The deep branch of the radial nerve enters the supinator muscle and innervates it.
- Turn the upper limb and look for the deep branch of the radial nerve where it emerges from the distal border of the supinator muscle . When the deep branch of the radial nerve emerges from the supinator muscle, its name changes to posterior interosseous nerve. The posterior interosseous nerve provides motor branches to the extensor muscles.
- Observe that the posterior interosseous nerve is accompanied by the posterior interosseous artery, which is a branch of the common interosseous artery. The posterior interosseous nerve supplies the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis muscles.
Dissection Review
- Replace the muscles of the posterior compartment of the forearm into their correct anatomical positions.
- Use the dissected specimen to review the attachments of the extensor tendons.
- Note that the tendons of three strong extensor muscles (extensor carpi radialis longus, extensor carpi radialis brevis, and extensor carpi ulnaris) attach to the proximal ends of metacarpal bones. These three extensors of the wrist work synergistically with the flexors of the digits: A firm grasp requires an extended wrist.
- Review the extensor expansion of digit 3. Recall the muscles that insert there and the action of each muscle.
- Review the course of the common interosseous branch of the ulnar artery and observe how the posterior interosseous artery enters the posterior compartment of the forearm.
- Review the course of the radial artery from the cubital fossa to the deep palmar arch.
- Palpate the anatomical snuffbox on yourself. Feel the pulsations of the radial artery within its boundaries.
- Recall the rule for innervation of the posterior compartment of the forearm:
- The radial nerve innervates all of the muscles in the posterior compartment of the forearm.
- Note that there are no intrinsic muscles in the dorsum of the hand. Therefore, there are no muscles in the hand that are innervated by the radial nerve.