PHARYNX AND LARYNX
Learning Objectives:
- Describe the musculature associated with the pharynx.
- Describe the nasopharynx, oropharynx, and laryngopharynx in terms of their locations, blood supplies and innervations.
- Identify and describe the cartilages that are related to the larynx.
- Identify and describe the membranes that are related to the larynx.
- Identify the various parts of the laryngeal inlet and cavity.
- Describe the nerves supplying the laryngeal mucosa.
- Describe the muscles associated with the larynx.
- Describe the nerves supplying the laryngeal muscles.
- Describe the arteries that supply the larynx.
- Visualize and relate structures of the larynx with respect to adjacent structures.
Examination of the cervical viscera will be conducted from a posterior approach. To facilitate this approach, the head must be detached from the vertebral column. The joints between the skull and the first cervical vertebra (craniovertebral joints) are the logical site for separation of the head from the vertebral column.
The retropharyngeal space will be opened from the base of the skull to the superior thoracic aperture. The ligaments of the craniovertebral joints will be cut. The atlanto-occipital joints (left and right) will be disarticulated and the prevertebral muscles will be cut where they cross the atlanto-occipital joints.
Osteology: Craniovertebral Joints
Refer to a skeleton and review the following:

- Atlas (C1)
- Anterior arch
- Superior articular facet
- Transverse process
- Posterior arch
- Anterior tubercle
- Axis (C2)
- Dens

- Occipital bone
- Occipital condyle
- Pharyngeal tubercle
- Foramen magnum
- Atlanto-occipital joint - between the occipital condyle and the superior articular facet of the atlas
- Transverse ligament of the atlas - holds the dens to the anterior arch of the atlas
Dissection Instructions: Retropharyngeal Space
- Review the structures that pass through the foramen magnum: brainstem, vertebral arteries (left and right), and cervical roots of the accessory nerves (left and right). Review the hypoglossal nerve (CN XII) where it enters the hypoglossal canal. Review the structures that enter the jugular foramen: glossopharyngeal nerve (CN IX), vagus nerve (CN X), accessory nerve (CN XI), and sigmoid sinus.
- Reflect the sternocleidomastoid muscle on both sides, taking care to separate each muscle from deeper structures all the way to the mastoid process.
- Insert the fingers of both hands posterior to the carotid sheaths (see Fig. 7.64, arrow). Push your fingers medially until they meet posterior to the cervical viscera. Your fingers are now in the retropharyngeal space. Tie a string around all of the cervical viscera at the level of the thyroid cartilage.
- To separate the viscera from the vertebral column, work your fingers superiorly as far as the basilar part of the occipital bone. This is the superior limit of the retropharyngeal space. Work your fingers inferiorly toward the superior thoracic aperture. Note that the retropharyngeal space extends into the thorax. On both sides, as superiorly as possible, tie another piece of string around the internal carotid artery, internal jugular vein, cranial nerves IX, X, XI and XII. These structures have to be preserved intact when disarticulating the skull.
- Turn the cadaver to the prone position. A wedge-shaped portion of the occipital bone was removed earlier (Fig. 7.65). Use bone cutters to remove the posterior arch of the atlas if it hasn't been removed already (Fig. 7.65). Open the spinal dura mater and remove any portion of the spinal cord that remains.
- Strip the dura mater from the anterior border of the foramen magnum and identify the tectorial membrane (Fig. 7.66). The tectorial membrane is continuous with the posterior longitudinal ligament. Superior to the anterior border of the foramen magnum, above the cervical nerve roots, cut the tectorial membrane and reflect it inferiorly as far as possible (Fig. 7.66).
- Anterior to the tectorial membrane, identify the cruciate ligament of the atlas (Fig. 7.66). The cruciate ligament has three parts: superior longitudinal band, transverse ligament of the atlas, inferior longitudinal band.
- Use a scalpel to cut the superior longitudinal band and the transverse ligament of the atlas. Retract the cruciate ligament and identify the left and right alar ligaments (Fig. 7.66). The alar ligaments extend from the dens to the lateral margins of the foramen magnum and they control lateral rotation and side-to-side movements of the head.
- Place a probe on the side of the dens under each alar ligament. Use a scalpel to cut the alar ligaments close to the dens. Note that the rotation of the head is now very easy and extensive if the alar ligaments have been completely cut.



Dissection Instructions: Disarticulation of the Head
- Use a scalpel to open the capsule of the atlanto-occipital joint on both sides (Fig. 7.65). Force a chisel into each atlanto-occipital joint and disarticulate it.
- Turn the cadaver to the supine position. Retract the cervical viscera and contents of the carotid sheath anteriorly.
- Identify the sympathetic trunk and the superior cervical sympathetic ganglion on the anterior surface of the cervical vertebral column. On the left side identify the internal carotid nerve, which passes from the superior end of the superior cervical ganglion to the internal carotid artery. Sever the internal carotid nerve just superior to the superior cervical ganglion and leave the sympathetic trunk attached to the vertebral column. On the right side, leave the internal carotid nerve intact and reflect the sympathetic trunk and the superior cervical ganglion with the head and cervical viscera.
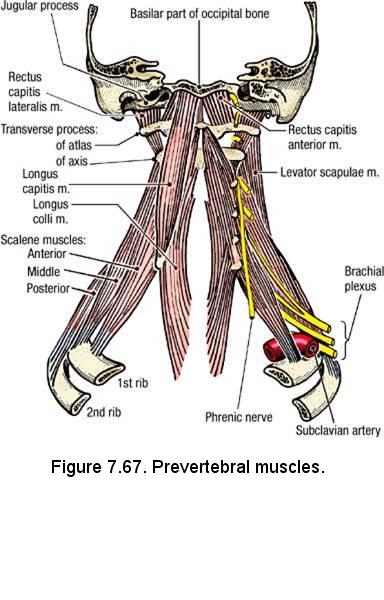
- Protect cranial nerves IX, X, XI, and XII where they emerge from the base of the skull near the internal jugular vein. All these structures were tied with a string. Insert a scalpel blade between the transverse process of the atlas and the occipital bone and sever the rectus capitis lateralis muscle on each side (Fig. 7.67). Repeat this cut on the opposite side of the neck (NOTE: These muscles are not easily identified- just be sure that you are protecting the cranial nerves exiting from the base of the skull and the contents of the carotid sheath when you cut soft tissue).
- More medially, sever the rectus capitis anterior and longus capitis muscles. Repeat this cut on the opposite side of the neck. Cut across the median plane just superior to the anterior arch of the atlas. Forcefully push the head anteriorly to detach it from the vertebral column.
- Inspect the base of the skull from the posterior perspective and look for remnants of the C1 vertebra attached to the atlanto-occipital joint. If remnants of the C1 vertebra are present, use bone cutters to remove them.
Dissection Instructions: Prevertebral and Lateral Vertebral Region
- On the anterior surface of the cervical vertebral column, examine the prevertebral fascia. The prevertebral fascia covers the prevertebral muscles (longus colli and longus capitis muscles) and the lateral vertebral muscles (anterior, middle, and posterior scalene muscles).
- Identify the longus colli, longus capitis, and anterior scalene muscles (Fig. 7.67). Review the contributions to the brachial plexus made by the ventral rami of spinal nerves C5 to C8.
- On the left side of the cervical vertebral column, study the sympathetic trunk running longitudinally on the prevertebral muscles. Identify the superior cervical ganglion, which is the cranial-most sympathetic ganglion and supplies the head.
- Follow the sympathetic trunk inferiorly and attempt to identify the middle and inferior cervical ganglia. These ganglia are not always obvious. Frequently, the inferior cervical ganglion is fused with the first thoracic ganglion to form the cervicothoracic (stellate) ganglion. You will not be asked to differentiate between an inferior cervical ganglion and a cervicothoracic (stellate) ganglion.
- Observe the gray rami communicantes that connect the sympathetic ganglia with the ventral rami of cervical spinal nerves.
- Follow the vertebral artery into the transverse foramen of vertebra C6 and observe where it emerges from the transverse foramen of the atlas (C1). Appreciate that the vertebral artery is well protected within the transverse foramina.
Dissection Review
- Use a skull to review the anatomy of the occipital bone.
- In the cadaver, review the structures that pass through the foramen magnum, hypoglossal canal, and jugular foramen.
- Use a skeleton to study the atlantoaxial and atlanto-occipital joints.
- Review the course of the sympathetic trunk from the upper thorax to the base of the skull.
- Review the origin and relationships of the roots of the brachial plexus.
Dissection Overview: Muscles of the Pharyngeal Wall
The airway crosses the digestive tract in the pharynx. The pharynx extends from the base of the skull to the inferior border of the cricoid
cartilage (vertebral level C6). The pharyngeal wall consists of three layers. From outside inward these layers are:
- Buccopharyngeal fascia - the adventitia of the pharynx that is continuous with the connective tissue that covers the buccinator muscle
- Muscular layer - composed of an outer circular part and an inner longitudinal part
- Mucous membrane
Dissection Instructions: Muscles of the Pharyngeal Wall
The order of dissection will be as follows: The external surface of the pharynx will be dissected from the posterior direction.
The pharyngeal plexus of nerves will be identified and the borders of the pharyngeal constrictor muscles will be defined.
The stylopharyngeus muscle and glossopharyngeal nerve will be identified. The contents of the carotid sheath will be examined and cranial
nerves IX, X, XI, and XII will be followed from the base of the skull to their regions of distribution. The sympathetic trunk will be studied.

- The cadaver should be in the supine position. Push the head anteroinferiorly and let the chin rest on the thorax. Use a probe to clean the buccopharyngeal fascia from the posterior surface of the pharynx.
- Identify the inferior pharyngeal constrictor muscle. The anterior attachments of the inferior pharyngeal constrictor muscle are the oblique line of the thyroid cartilage and the lateral surface of the cricoid cartilage (Fig. 7.68B). The posterior attachment of the inferior pharyngeal constrictor muscle is the pharyngeal raphe (Fig. 7.68A). Beginning near the thyroid cartilage, use blunt dissection to clean the superior border of the inferior pharyngeal constrictor muscle.
- Identify the middle pharyngeal constrictor muscle. The anterior attachments of the middle pharyngeal constrictor muscle are the greater horn of the hyoid bone and the inferior portion of the stylohyoid ligament (Fig. 7.68B). The posterior attachment of the middle pharyngeal constrictor muscle is the pharyngeal raphe. Note that the inferior part of the middle pharyngeal constrictor muscle lies deep to the inferior pharyngeal constrictor muscle. Use blunt dissection to clean the superior border of the middle pharyngeal constrictor muscle.
- Superior to the middle pharyngeal constrictor muscle, identify the superior pharyngeal constrictor muscle. The anterior attachment of the superior pharyngeal constrictor muscle is the pterygomandibular raphe and its posterior attachments are the pharyngeal raphe and pharyngeal tubercle of the occipital bone (Fig. 7.68A). Note that the inferior part of the superior pharyngeal constrictor muscle lies deep to the middle pharyngeal constrictor muscle.
- Use blunt dissection to define the superior border of the superior pharyngeal constrictor muscle. The pharyngobasilar fascia is the dense connective tissue membrane that attaches the superior edge of the superior pharyngeal constrictor muscle to the base of the skull.
- The stylopharyngeus muscle is attached to the medial surface of the styloid process superiorly and to the inner aspect of the pharyngeal wall inferiorly. It enters the pharyngeal wall by passing between the superior and middle pharyngeal constrictor muscles (Fig. 7.68A).
- To find the stylopharyngeus muscle, first palpate the greater horn of the hyoid bone. One finger's width above the greater horn of the hyoid bone, use blunt dissection to find the stylopharyngeus muscle where it passes between the superior pharyngeal constrictor muscle and the middle pharyngeal constrictor muscle.
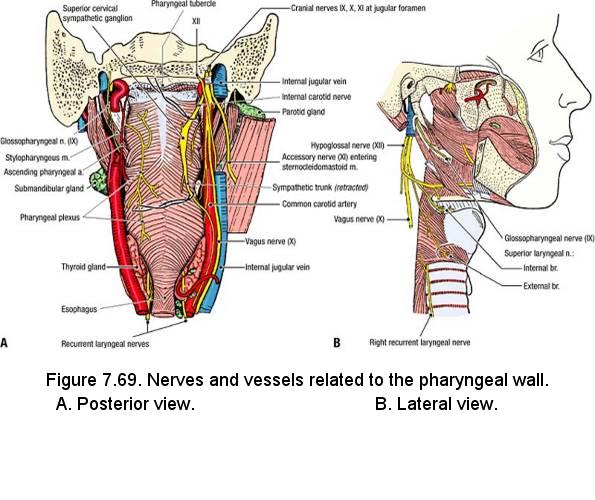
- Use a probe to clean the posterior and lateral surfaces of the stylopharyngeus muscle. Identify the glossopharyngeal nerve (CN IX) that crosses the posterior and lateral surfaces of the stylopharyngeus muscle to enter the pharynx (Fig. 7.69A).
- Examine the inferior part of the inferior constrictor muscle (Fig. 7.69B). Note that the most inferior fibers of the inferior constrictor muscle are continuous with the circular fibers of the esophagus.
- Identify the pharyngeal plexus of nerves (Fig. 7.69A). The pharyngeal plexus is located on the posterolateral aspect of the pharynx. Note that the pharyngeal plexus receives branches from the:
- Glossopharyngeal nerve - sensory to the pharyngeal mucosa
- Vagus nerve - motor to the pharyngeal constrictor muscles
- Superior cervical sympathetic ganglion - vasomotor
- Identify the contents of the carotid sheath from the posterior view (Fig. 7.69A). Follow the internal carotid artery superiorly as far as possible. Note that the internal jugular vein is lateral to the internal carotid artery.
- Identify the glossopharyngeal nerve (CN IX), vagus nerve (CN X), and accessory nerve (CN XI) where they exit the jugular foramen medial to the internal jugular vein (Fig. 7.69A):
- Glossopharyngeal nerve (CN IX) - passes between the internal and external carotid arteries as it approaches the stylopharyngeus muscle.
- Vagus nerve - lies posterior to the internal carotid artery and internal jugular vein in the carotid sheath. Trace the vagus nerve from the base of the skull to the thorax. The superior laryngeal nerve arises from the vagus nerve about 2.5 cm inferior to the base of the skull. Trace the branches of the superior laryngeal nerve (internal and external branches of the superior laryngeal nerve) to the larynx (Fig. 7.69B). The pharyngeal branch of the vagus nerve arises near the base of the skull. Follow the pharyngeal branch to the pharyngeal plexus.
- Accessory nerve (CN XI) - usually passes between the internal jugular vein and the internal carotid artery to reach the deep surface of the sternocleidomastoid muscle (Fig. 7.69A).
- Identify the hypoglossal nerve (CN XII) in the submandibular triangle and follow it posteriorly and superiorly as far as the base of the skull (Fig. 7.69B). Note that the hypoglossal nerve passes lateral to the internal and external carotid arteries.
- On the right side of the cadaver, verify that the superior cervical sympathetic ganglion and the sympathetic trunk are posterior and medial to the carotid sheath (Fig. 7.69A). Identify the internal carotid nerve that passes from the superior end of the superior cervical ganglion to the internal carotid artery.
Dissection Overview: Bisection of the Head
- Use a scalpel to cut the posterior wall of the pharynx in the midline. Start at the superior end of the esophagus and cut through the pharyngeal raphe up to the pharyngeal tubercle.
- Use a scalpel to divide the uvula and the soft palate in the median plane.
- Turn the specimen and use a scalpel to cut through the upper lip in the midline.
- The skull must be sawed just lateral to the median plane. The nasal septum may not be in the median plane, so you must examine each nasal cavity and decide on which side the saw cut should be made in order to avoid the nasal septum.
- On the chosen side, use a scalpel to cut through the cartilages of the external nose parallel to the nasal septum.
- Examine a skull and study the bones through which you must cut:
- Nasal bone and frontal bone
- Cribriform plate of the ethmoid bone
- Body of the sphenoid bone
- Hard palate
- Basilar part of the occipital bone as far as the foramen magnum
- Saw through the skull from superior to inferior. Begin lateral to the crista galli (the side of the saw blade should touch the crista galli) and keep the blade close to the nasal septum. Cut through the nasal and frontal bones, ethmoid bone, body of the sphenoid, dorsum sellae, basilar part of the occipital bone, and hard palate. Stop when the saw has passed into the foramen magnum. Do not cut the tongue or mandible at this time.
- The two superior halves of the head should separate from each other. The tongue should be exposed.
Dissection Overview: Internal Aspect of the Pharynx
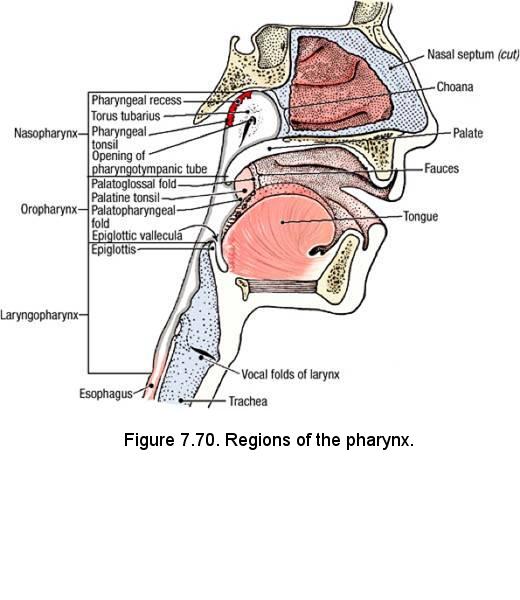
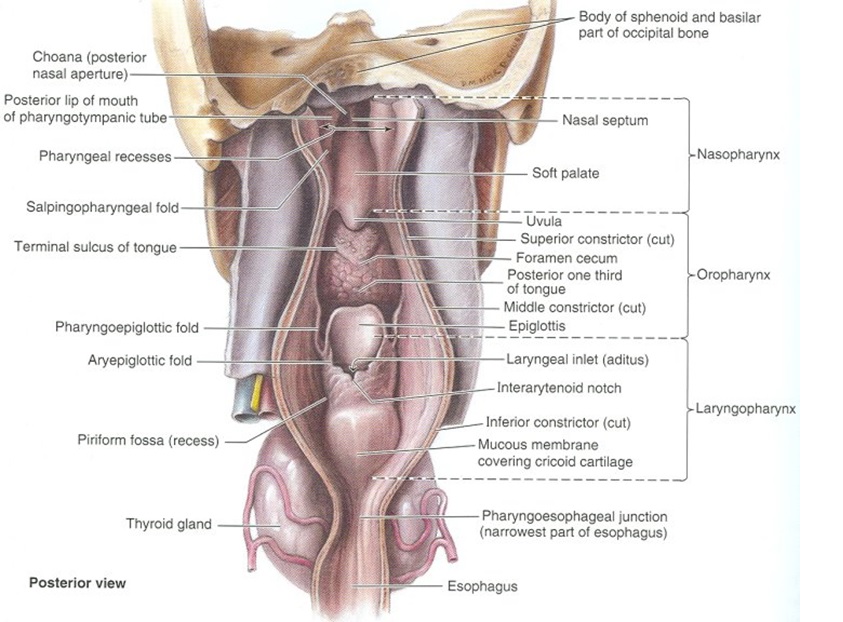
- The lumen of the pharynx communicates anteriorly with three cavities: nasal, oral, and larynx (Fig. 7.70). Identify the parts of the pharynx: nasopharynx, oropharynx, and laryngopharynx (Fig. 7.70 and figure showing posterior view of opened pharynx).
- The nasopharynx lies posterior to the nose and superior to the soft palate (Fig. 7.70). Identify the posterior nasal aperture (choana) that is the transition region from the nasal cavity to the nasopharynx. The choanae of the two sides are separated by the posterior end of the nasal septum.
- On the lateral wall of the nasopharynx, identify the opening of the pharyngotympanic tube (auditory tube, eustachian tube).
- Superior to the opening of the pharyngotympanic tube, identify the torus tubarius, which is the cartilage of the pharyngotympanic tube that is covered by mucosa (Fig. 7.70). The salpingopharyngeal fold extends posteroinferiorly from the torus tubarius.
- Superior and posterior to the torus tubarius, identify the pharyngeal recess. The pharyngeal tonsil (adenoid) is located in the mucous membrane above the pharyngeal recess.
- The oropharynx lies posterior to the oral cavity. It is bounded superiorly by the soft palate and extends inferiorly to the level of the epiglottis (Fig. 7.70).
- In the oropharynx, identify the palatoglossal fold. The palatoglossal fold forms a dividing line between the oral cavity and the oropharynx. The transitional region between the right and left palatoglossal folds is called the fauces.
- Identify the palatopharyngeal fold, which is posterior to the palatoglossal fold. The palatopharyngeal fold descends along the lateral wall of the oropharynx. Between the palatoglossal fold and the palatopharyngeal fold is the palatine tonsil. Use a mirror to identify the palatine tonsil on yourself.
- The laryngopharynx lies posterior to the larynx. This portion of the pharynx extends from the hyoid bone to the lower border of the cricoid cartilage (Fig. 7.70).
- In the midline of the laryngopharynx, identify the epiglottis and the laryngeal inlet (aditus) of the larynx. Farther inferiorly, identify the piriform recess, which is lateral to the midline. The borders of the piriform recess are:
- Medial - larynx
- Lateral - thyroid cartilage
- Posterior - inferior pharyngeal constrictor muscle
IN THE CLINIC: Adenoids
Enlarged pharyngeal tonsils are called adenoids. Adenoids obstruct the flow of air from the nose through the nasopharynx, making mouth breathing necessary.
Enlarged pharyngeal tonsils are called adenoids. Adenoids obstruct the flow of air from the nose through the nasopharynx, making mouth breathing necessary.
Dissection Overview: Internal Aspect of the Larynx
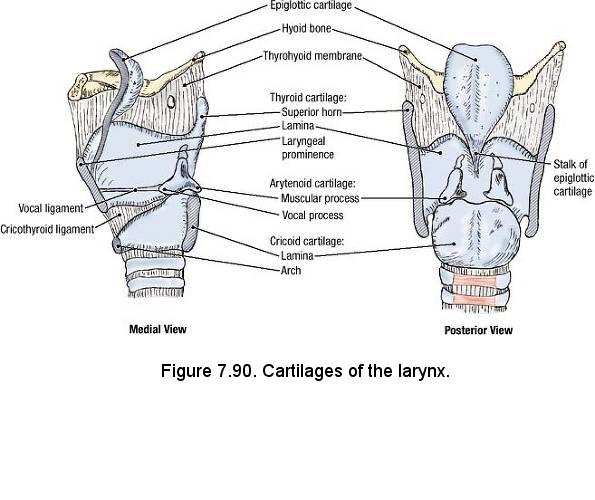
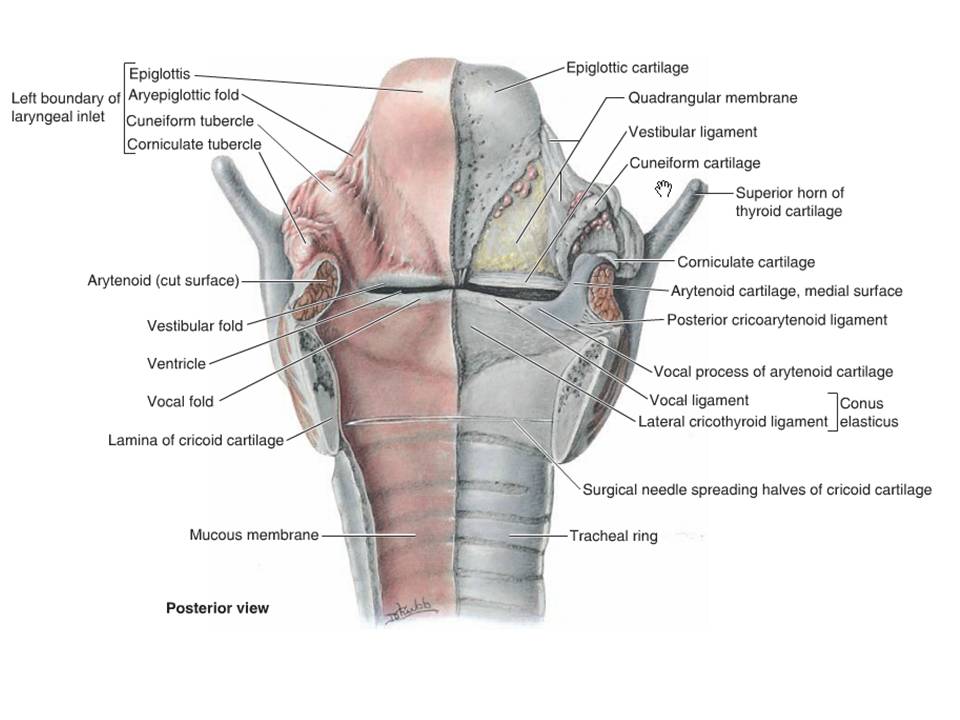
- From your atlas and available models, study the cartilages that compose the laryngeal skeleton (Fig. 7.90). These include the epiglottic, cricoid, thyroid, arytenoid, corniculate and cuneiform cartilages
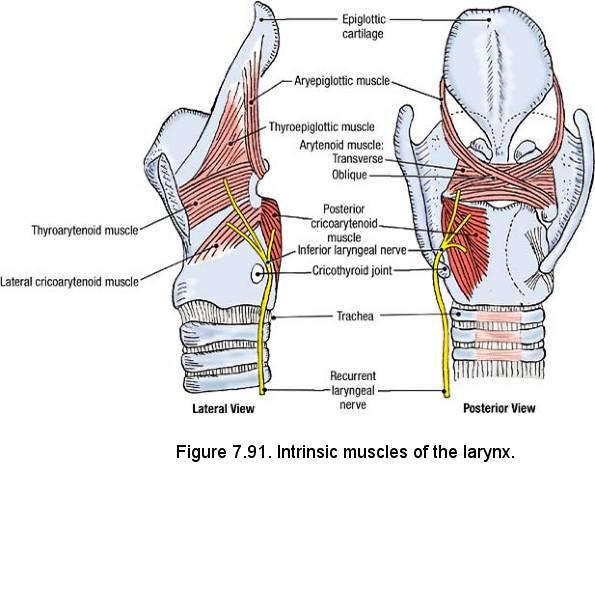
- Refer to Fig. 7.91. Strip the mucosa from the entire pharyngeal aspect of the larynx to expose the posterior cricoarytenoid muscles (proximal attachment is the lateral margin and the posterior lamina of the cricoid cartilage and the distal attachments are the muscular processes of the arytenoid cartilages) and the arytenoid muscle (this muscle attaches to both arytenoid cartilages and has transverse and oblique fibers).
- Use scissors and cut through the arytenoid muscle, the lamina of the cricoid cartilage, and the trachea in the median plane.
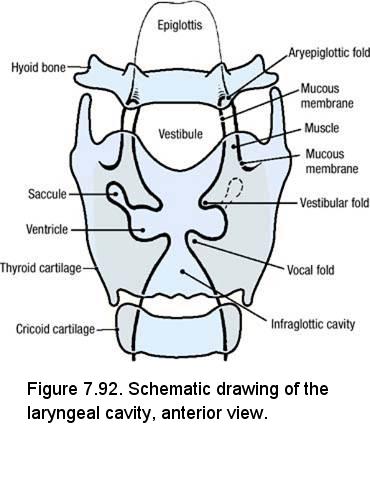
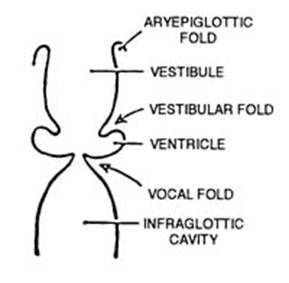
- Open the larynx and observe that the larynx has three spaces or cavities: the vestibule, ventricle and infraglottic cavity (See Figs. 7.92 and schematic below).
- Examine the interior of the larynx from the superior aspect and note that the vestibular (false vocal) folds lie superolateral to the vocal (true vocal) folds or cords. The rima glottidis is the space between the true vocal folds.
- Remove the mucous membrane from one half of the interior of the larynx between the cricoid cartilage and the vocal ligament. This reveals the conus elasticus or (lateral) cricothyroid ligament. The thickened upper margin of the conus elasticus forms the vocal ligament.
- The aryepiglottic folds bound the upper border of the laryngeal inlet. Use something to scrape the mucosa from the inner surface of the aryepiglottic fold and uncover the quadrangular membrane. Observe that this membrane extends from the lateral border of the epiglottic cartilage to the arytenoid cartilage and that it becomes thickened inferiorly to help form the vestibular fold.
- The cricothyroid joint is a synovial joint that is reinforced by short ligaments. Observe that the recurrent laryngeal nerve enters the larynx by passing posterior to the cricothyroid joint (Fig. 7.91). At this point, the name of the recurrent laryngeal nerve changes to the inferior laryngeal nerve.
- Sensory innervation to the mucosa that lines the interior of the larynx below and including the vocal folds is derived from the recurrent laryngeal nerve, whereas the mucosa above the vocal folds is supplied by the internal branch of the superior laryngeal nerve.
- Along the lateral border of the thyrohyoid membrane, again find the internal branch of the superior laryngeal nerve and the superior laryngeal artery. Trace the internal branch of the superior laryngeal nerve through the thyrohyoid membrane for a short distance into the inner mucosa of the larynx. Recall that the superior laryngeal nerve (of the vagus nerve) gives rise to both an internal and external branch, and that the latter descends to supply the cricothyroid muscle.
- Trace the superior laryngeal artery back to its origin from the superior thyroid artery and note that this artery enters the larynx by penetrating the thyrohyoid membrane.
Dissection Review
- Review the attachments, innervation, and action of the pharyngeal constrictor muscles.
- Use a textbook description and the cadaver to review the pharyngeal plexus.
- Trace each of the following cranial nerves from the posterior cranial fossa to its area of distribution: glossopharyngeal (CN IX), vagus (CN X), accessory (CN XI), and hypoglossal (CN XII).
- Review the relationships of the contents of the carotid sheath.
- Review the boundaries and contents of each part of the pharynx.
- Replace the head and larynx in their correct anatomical positions.
- Use a cross-sectional drawing of the neck and the dissected specimen to review the relationship of the larynx to the vertebral column, carotid sheaths, and other cervical viscera.
- Trace the right and left vagus nerves into the thorax and follow the right and left recurrent laryngeal nerves from the thorax to the larynx. Note the differences.
- Review the branches of the external carotid artery.
- Follow the superior thyroid artery to the thyroid gland and review the course of the superior laryngeal artery as it passes through the thyrohyoid membrane to enter the larynx. Recall that the superior laryngeal artery courses with the internal branch of the superior laryngeal nerve.
- Review the course of the superior laryngeal nerve from the vagus nerve to its bifurcation. Follow the external laryngeal branch to the cricothyroid muscle.
- Use the dissected specimen to review the attachments and action of each intrinsic laryngeal muscle that was identified during dissection.
- Review the movements of the vocal folds during phonation, quiet breathing, and rapid breathing.
NASAL AND ORAL CAVITIES
Learning Objectives (including prosection of pterygopalatine fossa):
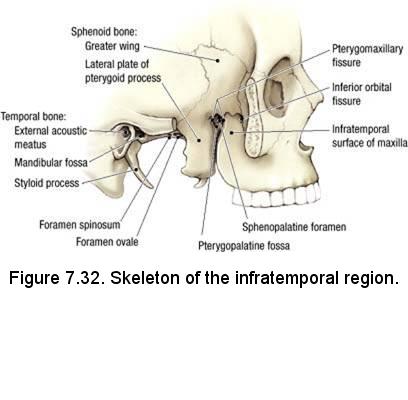
- Identify and describe the bony skeleton of the nasal cavity and pterygopalatine fossa.
- Identify and describe the blood vessels and nerves supplying the nasal cavity.
- Identify and describe the structures related to the nasal cavity and pterygopalatine fossa.
- Identify the bony openings into the pterygopalatine fossa.
- Describe the pathways for nerve fibers and blood vessels that pass through the pterygopalatine fossa.
- Describe the pathways for fibers that pass through or synapse in the pterygopalatine ganglion.
- Describe the hard and soft palates.
- Identify the muscles associated with the soft palate.
- Describe the nerve supply to the muscles and mucosa of the hard and soft palates.
- Identify the musculature of the tongue.
- Identify the nerves and vessels supplying the mucosa and musculature of the tongue.
- Identify and visualize the muscles of the floor of the mouth and their nerve supply.
- Visualize the structures of the sublingual area.
- Identify the nerves that pass through or synapse in the submandibular ganglion.
There are two nasal cavities: Right and left. The nostril (naris) is the anterior entrance to the nasal cavity. Posteriorly, the nasal cavity opens into the nasopharynx through the choana. The nasal cavity is lined by mucosa that is attached directly to bones and cartilages. The bones and cartilages give the walls of the nasal cavity their characteristic contours. The superior one-third of the nasal mucosa is olfactory in nature and the remainder is respiratory in nature. The nasal mucosa is highly vascular and capable of engorgement.
The order of dissection will be as follows: The nose and nasal cartilages will be studied. The nasal septum will be examined and removed. The features of the lateral nasal wall will be studied. The openings of the paranasal sinuses will be identified. The maxillary sinus will be opened and examined. The palatine canal, pterygopalatine fossa, and pterygopalatine ganglion will be viewed from the medial aspect via prosection. The nerves and vessels of the nasal cavity and palate will be summarized.
Osteology
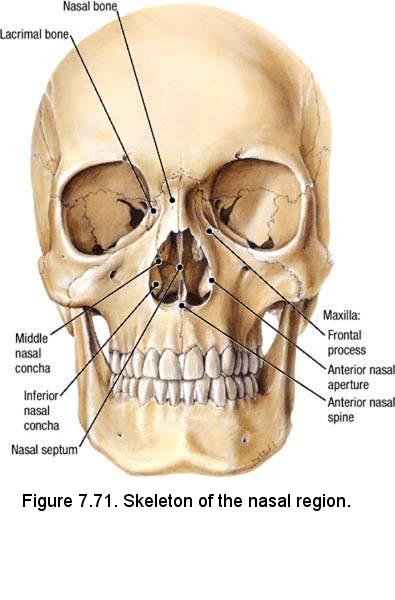
- Nasal bone
- Lacrimal bone
- Maxilla
- Frontal process
- Anterior nasal aperture
- Anterior nasal spine
- Nasal septum - bony part
- Middle nasal concha - part of the ethmoid bone
- Inferior nasal concha
Use an illustration to identify the bony features of the lateral nasal wall (Fig. 7.72):
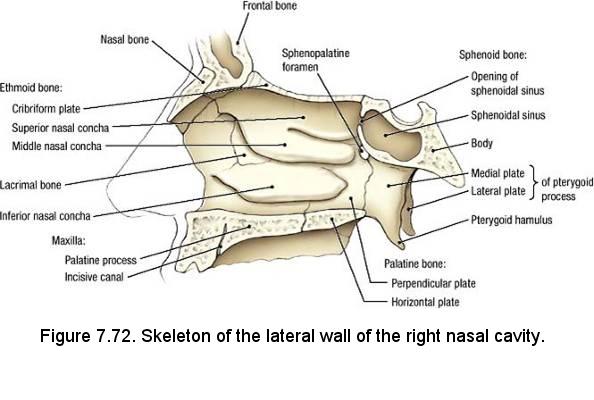
- Ethmoid bone
- Cribriform plate
- Superior nasal concha
- Middle nasal concha
- Lacrimal bone
- Inferior nasal concha
- Maxilla
- Palatine process
- Incisive canal
- Sphenoid bone
- Opening of the sphenoidal sinus
- Sphenoidal sinus
- Body
- Medial plate of the pterygoid process
- Lateral plate of the pterygoid process
- Palatine bone
- Perpendicular plate
- Horizontal plate
- Sphenopalatine foramen
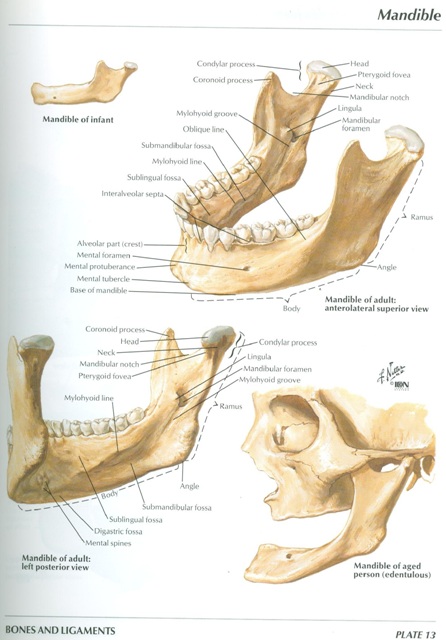
- Mylohyoid line
- Submandibular fossa
- Sublingual fossa
- Mylohyoid groove
- Digastric fossa
- Superior mental spines
- Inferior mental spines
External Nose

- On the cadaver, palpate the nasal bone. Inferior to the nasal bone palpate the lateral nasal cartilage (Fig. 7.73). The lateral nasal cartilage gives shape to the bridge of the nose.
- The lateral nasal cartilage is an extension of the septal cartilage. The septal cartilage separates the right and left nasal cavities and forms the anterior part of the nasal septum.
- Lateral to the septal cartilage is the alar cartilage (Fig. 7.73). The alar cartilage gives shape to the nostril.
Nasal Cavity
- Examine the boundaries of the nasal cavity:
- Roof - a narrow region bounded by the nasal septum and by parts of three other bones: nasal bone, cribriform plate of ethmoid bone, and sphenoid bone
- Floor - palatine process of the maxilla and horizontal plate of the palatine bone
- Medial wall - nasal septum
- Lateral wall - maxilla, lacrimal bone, ethmoid bone, inferior nasal concha, and perpendicular plate of the palatine bone
- In the cadaver, observe that the bones and cartilages of the nasal cavity are obscured by the mucosa that covers them. The vessels and nerves of the nasal cavity are contained within this mucosa.
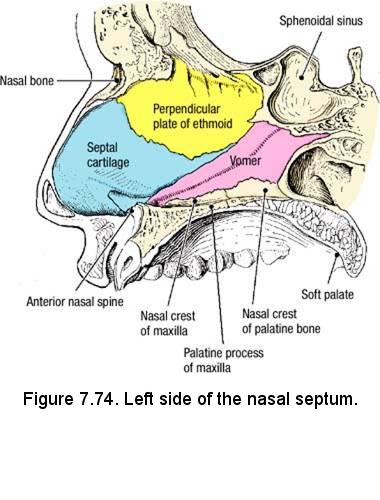
- Examine the half of the head that contains the nasal septum. Strip the mucosa completely off of the nasal septum and identify the perpendicular plate of the ethmoid bone, vomer, and septal cartilage (Fig. 7.74).
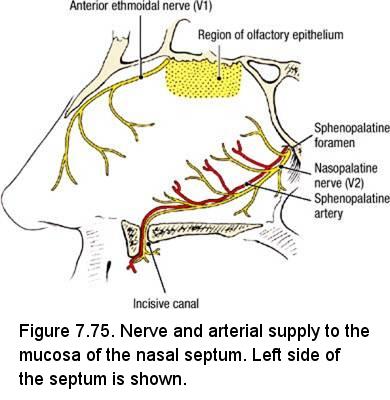
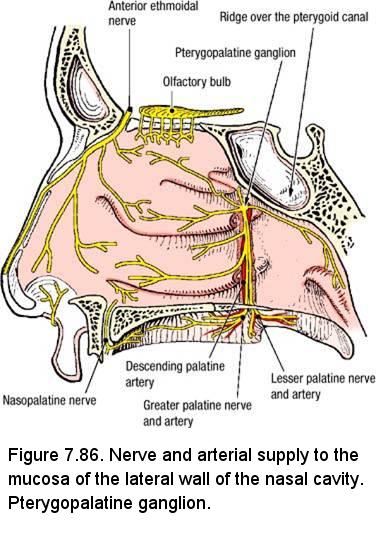
- Use a probe and forceps to remove the bony and cartilaginous parts of the nasal septum. Leave intact the mucosa that lines the other side of the nasal septum. In the mucosa of the nasal septum, identify the nasopalatine nerve and the sphenopalatine artery (Fig. 7.75). Note that the nasopalatine nerve and the sphenopalatine artery pass diagonally down the nasal septum from the sphenopalatine foramen to the incisive canal. In addition to the nasal septum, the nasopalatine nerve and sphenopalatine artery supply a portion of the oral mucosa that covers the hard palate.
- Note that the mucosa near the cribriform plate is the olfactory area (Fig. 7.75). The olfactory area also extends down the lateral wall of the nasal cavity for a short distance.
- Save the nasal septum for review.
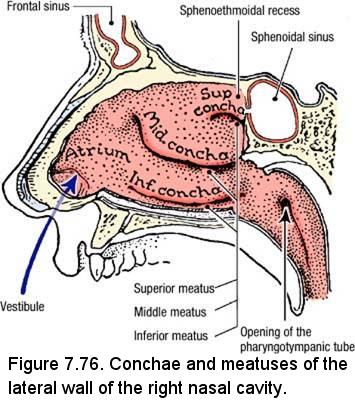
- On the side that does not contain the nasal septum, inspect the lateral wall of the nasal cavity (Fig. 7.76). Identify:
- Sphenoethmoidal recess - above the superior concha
- Superior concha
- Superior meatus - inferior to the superior concha
- Middle concha
- Middle meatus - inferior to the middle concha
- Inferior concha
- Inferior meatus - inferior to the inferior concha
- Vestibule - the area superior to the nostril and anterior to the inferior meatus
- Atrium - the area superior to the vestibule and anterior to the middle meatus
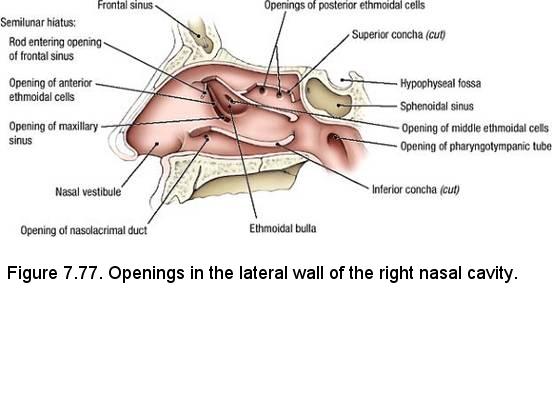
- Use scissors to transect the anterior ⅔ of the inferior concha, leaving the posterior ⅓ attached as a hinge. Identify the opening of the nasolacrimal duct (Fig. 7.77).
- Use scissors to transect the anterior ⅔ of the middle concha, leaving the posterior ⅓ attached as a hinge. In the middle meatus identify a curved slit, the semilunar hiatus (hiatus semilunaris) (Fig. 7.77). Posterior to the curvature of the semilunar hiatus, identify the ethmoidal bulla (bulla ethmoidalis).
- Within the semilunar hiatus, identify (Fig. 7.77):
- Opening of the frontal sinus
- Opening of the anterior ethmoidal cells
- Opening of the maxillary sinus
- Identify the opening of the middle ethmoidal cells on the summit of the ethmoidal bulla.
- Identify the opening of the posterior ethmoidal cells in the superior meatus. Note that the openings of the ethmoid air cells may be too small to see.
- Identify the opening of the sphenoidal sinus in the sphenoethmoidal recess. Note that the opening of the sphenoidal sinus may be too small to see.
- Examine the sphenoidal sinus (Fig. 7.77). The sphenoidal sinus is a paired structure that is lined by mucosa that is continuous with the mucosa of the nasal cavity. Note that the sphenoidal sinus lies directly inferior to the hypophyseal fossa and pituitary gland.
- Note that the ethmoidal cells are located between the nasal cavity and the orbit (Figs. 7.78 and 7.79). The ethmoidal cells may be observed from the superior perspective by reviewing the dissection of the orbit that was completed previously.
- The maxillary sinus is a three-sided pyramid with an average adult capacity of 15 mL. Observe an illustration of a coronal section through the maxillary sinus and note the following (Fig. 7.79):
- The roof of the maxillary sinus is the floor of the orbit and the infraorbital nerve innervates the mucosa of the maxillary sinus.
- The floor of the maxillary sinus is the alveolar process of the maxilla.
- The opening of the maxillary sinus is near its roof.
- The roots of the maxillary teeth may project into the maxillary sinus.


IN THE CLINIC: Sphenoidal Sinus
Surgical approaches to the pituitary gland take advantage of the fact that the sphenoidal sinus and nasal cavity provide a direct approach.
Surgical approaches to the pituitary gland take advantage of the fact that the sphenoidal sinus and nasal cavity provide a direct approach.
IN THE CLINIC: Maxillary Sinus
When the head is in the upright position, the maxillary sinus cannot drain. If infections of the maxillary sinus persist, an opening was sometimes made surgically through the inferior meatus near the floor of the maxillary sinus to promote drainage. Due to low effectiveness, this procedure is no longer performed.
When the roots of maxillary teeth project into the maxillary sinus, they are covered only by mucosa. During extraction of a maxillary molar or premolar tooth, the mucosa superior to the projecting root may be torn. As a result, a fistula may be formed between the oral cavity and the maxillary sinus.
When the head is in the upright position, the maxillary sinus cannot drain. If infections of the maxillary sinus persist, an opening was sometimes made surgically through the inferior meatus near the floor of the maxillary sinus to promote drainage. Due to low effectiveness, this procedure is no longer performed.
When the roots of maxillary teeth project into the maxillary sinus, they are covered only by mucosa. During extraction of a maxillary molar or premolar tooth, the mucosa superior to the projecting root may be torn. As a result, a fistula may be formed between the oral cavity and the maxillary sinus.
Dissection Overview: Oral Cavity
The oral region includes the oral cavity and its contents (teeth, gums, and tongue), the palate, and the part of the oropharynx that contains
the palatine tonsils. The oral cavity consists of:
- Oral vestibule - bounded externally by the lips and cheeks and internally by the teeth and gums.
- Oral cavity proper - the area between the alveolar arches and teeth. The largest content of the oral cavity proper is the tongue.
Dissection Instructions: Oral Cavity

- Inspect the tongue in the cadaver specimen. Identify (Fig. 7.87):
- Root - the posterior one-third
- Body - the anterior two-thirds
- Apex
- Dorsum
- Terminal sulcus (sulcus terminalis) - divides the anterior two-thirds from the posterior one-third
- Lingual tonsil - posterior to the terminal sulcus
- Foramen cecum - in the midline at the point of the terminal sulcus
- Median sulcus
- Lingual papillae - four types: vallate, filiform, fungiform, and foliate
- Note that the body of the tongue lies horizontally in the oral cavity and the root of the tongue lies more vertically. The root of the tongue constitutes the lower part of the anterior boundary of the oropharynx.
- At the root of the tongue (Fig. 7.87), identify:
- Median glossoepiglottic fold - a midline fold of mucosa between the dorsum of the tongue and the epiglottis
- Lateral glossoepiglottic fold - between the dorsum of the tongue and the lateral border of the epiglottis
- Epiglottic vallecula - a depression between median and lateral glossoepiglottic folds
- Use a new scalpel blade. Turn the specimen to expose the submental triangle.
- Use the scalpel to cut the mylohyoid muscles along their median raphe. Use a probe to separate the mylohyoid muscles from deeper structures.
- Identify the geniohyoid muscle, which is deep to the mylohyoid muscle. The anterior attachment of the geniohyoid muscle is the inferior mental spine of the mandible and its posterior attachment is the body of the hyoid bone. The geniohyoid muscle pulls the hyoid bone anteriorly.
- Use blunt dissection to separate the geniohyoid muscles in the midline. Use a saw to cut through the mandible in the median plane. Do not allow the saw to pass between the genioglossus muscles on the deep side of the mandible.
- Do not bisect the epiglottis, the hyoid bone, or the larynx at this time. Use a scalpel to bisect the tongue in the median plane, beginning at the apex and proceeding toward the epiglottis. Cut as far inferiorly as the hyoid bone.
- On the sectioned surface of the tongue, identify the genioglossus muscle. The anterior attachment of the genioglossus muscle is the superior mental spine of the mandible and its posterior attachment is the tongue. The genioglossus muscle protrudes the tongue. The genioglossus muscle is innervated by the hypoglossal nerve (CN XII).
- Use the cadaver specimen to review the sublingual features that were identified in your oral cavity:
- Frenulum of the tongue
- Sublingual fold
- Sublingual caruncle
- Opening of the submandibular duct
- Use a probe and forceps to carefully peel off the mucous membrane from the medial surface of the mandible. Start at the frenulum of the tongue and stop near the second mandibular molar tooth.
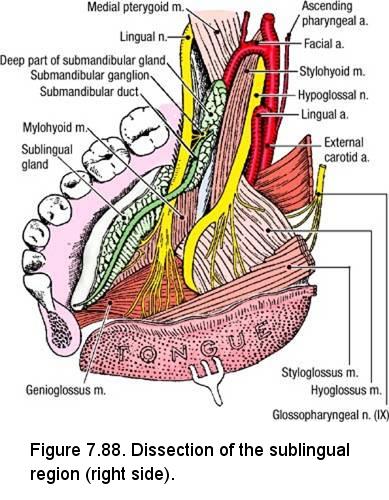
- Identify the sublingual gland immediately deep to the mucosa (Fig. 7.88). The sublingual gland rests on the mylohyoid muscle. The sublingual gland has about 12 short ducts that drain along the summit of the sublingual fold.
- Use a probe to dissect along the medial side of the sublingual gland and find the submandibular duct (Fig. 7.88). Follow the submandibular duct anteriorly to its opening on the sublingual caruncle. Use a probe to trace the submandibular duct posteriorly to the deep part of the submandibular gland (deep part). Note that the submandibular gland (deep part) is located on the deep side of the mylohyoid muscle.
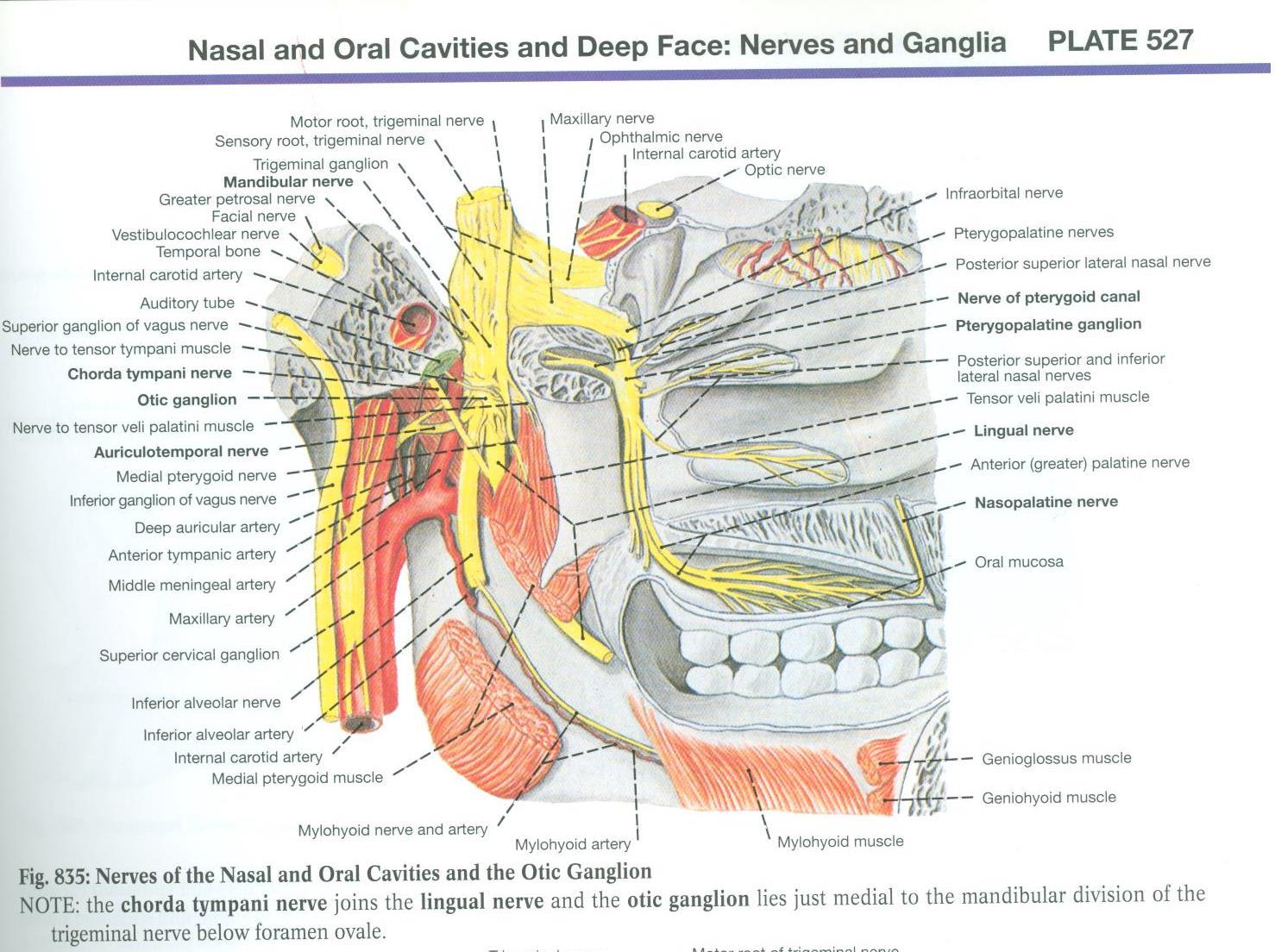
- Turn the specimen to expose the infratemporal fossa. Find the lingual nerve and trace it into the sublingual region of the oral cavity. Observe that the lingual nerve passes lateral, inferior, and medial to the submandibular duct (Fig. 7.88). The lingual nerve has several branches that supply the mucosa of the anterior two-thirds of the tongue with general sensation and taste fibers.
- Near the third mandibular molar tooth, identify the submandibular ganglion that is suspended below the lingual nerve. Read a textbook description of the parasympathetic function of the submandibular ganglion.
- Turn the specimen so that the submandibular triangle is exposed. Find the hypoglossal nerve (CN XII) and use a probe to trace it into the sublingual region. Note that the hypoglossal nerve passes between the submandibular gland and the hyoglossus muscle (Fig. 7.88). Observe that both the hypoglossal nerve and the lingual nerve pass between the hyoglossus muscle and the mylohyoid muscle to enter the sublingual region. The course of the hypoglossal nerve is inferior to the course of the lingual nerve.
- Identify the hyoglossus muscle, which is deep to the mylohyoid muscle (Fig. 7.89). The inferior attachments of the hyoglossus muscle are the body and greater horn of the hyoid bone and its superior attachment is the lateral side of the tongue. The hyoglossus muscle depresses and retracts the tongue.
- Near the superior end of the hyoglossus muscle, identify the styloglossus muscle (Fig. 7.89). The proximal attachment of the styloglossus muscle is the styloid process and its distal attachment is the lateral side of the tongue. The styloglossus muscle retracts the tongue and draws it superiorly.
- Return to the carotid triangle and locate the lingual artery where it arises from the external carotid artery (Fig. 7.89). Follow the lingual artery until it passes medial to the hyoglossus muscle where its name changes to deep lingual artery.
- The intrinsic muscles of the tongue and the three extrinsic muscles of the tongue (styloglossus, genioglossus, and hyoglossus) are innervated by the hypoglossal nerve (CN XII).

IN THE CLINIC: Hypoglossal Nerve
The genioglossus muscle protrudes the tongue. If one genioglossus muscle does not function (hypoglossal nerve dysfunction on that side), the tongue cannot be protruded in the midline. The functional side of the tongue protrudes normally and the side with the dysfunctional nerve is protruded less or not at all. Therefore, in testing for hypoglossal nerve lesions, the protruded tongue deviates toward the side of the nerve lesion.
The genioglossus muscle protrudes the tongue. If one genioglossus muscle does not function (hypoglossal nerve dysfunction on that side), the tongue cannot be protruded in the midline. The functional side of the tongue protrudes normally and the side with the dysfunctional nerve is protruded less or not at all. Therefore, in testing for hypoglossal nerve lesions, the protruded tongue deviates toward the side of the nerve lesion.
Dissection Review
- Use an illustration and the dissected specimen to review the features of the lateral wall of the nasal cavity.
- Review the relationship of the paranasal sinuses to the orbit, anterior cranial fossa, and nasal cavity.
- Review the drainage point of each paranasal sinus. Use the dissected specimen and an illustration to reconstruct the branching pattern of the maxillary division of the trigeminal nerve. Use a skull and the dissected specimen to follow the maxillary division from the trigeminal ganglion through the foramen rotundum, pterygopalatine fossa, and inferior orbital fissure to the infraorbital groove.
- Review the distribution of the following branches of the maxillary division of the trigeminal nerve: greater palatine, lesser palatine, nasopalatine, and infraorbital nerves.
- Review the surface features of the tongue.
- Review the innervation of the lingual mucosa.
- Follow the submandibular duct from the submandibular triangle to the sublingual caruncle.
- Trace the lingual nerve from the infratemporal fossa to the tongue. Note the relationship of the lingual nerve to the submandibular duct, hyoglossus muscle, and mylohyoid muscle.
- Review the chorda tympani and the role that it plays in sensory innervation of the tongue and parasympathetic innervation of the submandibular and sublingual glands.
- Locate the submandibular ganglion and state its function.
- Trace the hypoglossal nerve from the base of the skull to the tongue, noting its relationships to arteries and muscles.
- Organize the muscles of the tongue into extrinsic and intrinsic groups. State the attachments, innervation, and action of each extrinsic muscle.
- Use an illustration and the dissected specimen to review the origin and course of the facial and lingual arteries.
PROSECTION ASSIGNMENT: PTERYGOPALATINE FOSSA
- Use an illustration to study the following branches of the sphenopalatine artery:
- Posterior lateral nasal artery - to the lateral nasal wall
- Posterior septal branch - to the nasal septum
- The mucosa from the posterior part of the lateral nasal wall has been removed.
- On the prosection with the lateral wall of the nasal cavity intact, identify the sphenopalatine foramen (Fig. 7.85).
- Examine the side in which the lateral wall of the nasal cavity (the medial wall of the pterygopalatine fossa) has been removed to expose the contents of the greater palatine canal.
- Identify the greater palatine nerve, the lesser palatine nerve, and the descending palatine artery in the greater palatine canal (Fig. 7.86). The descending palatine artery is one of the terminal branches of the maxillary artery.
- At the inferior end of the greater palatine canal, note that the descending palatine artery divides to give rise to the greater palatine artery and the lesser palatine artery (Fig. 7.86).
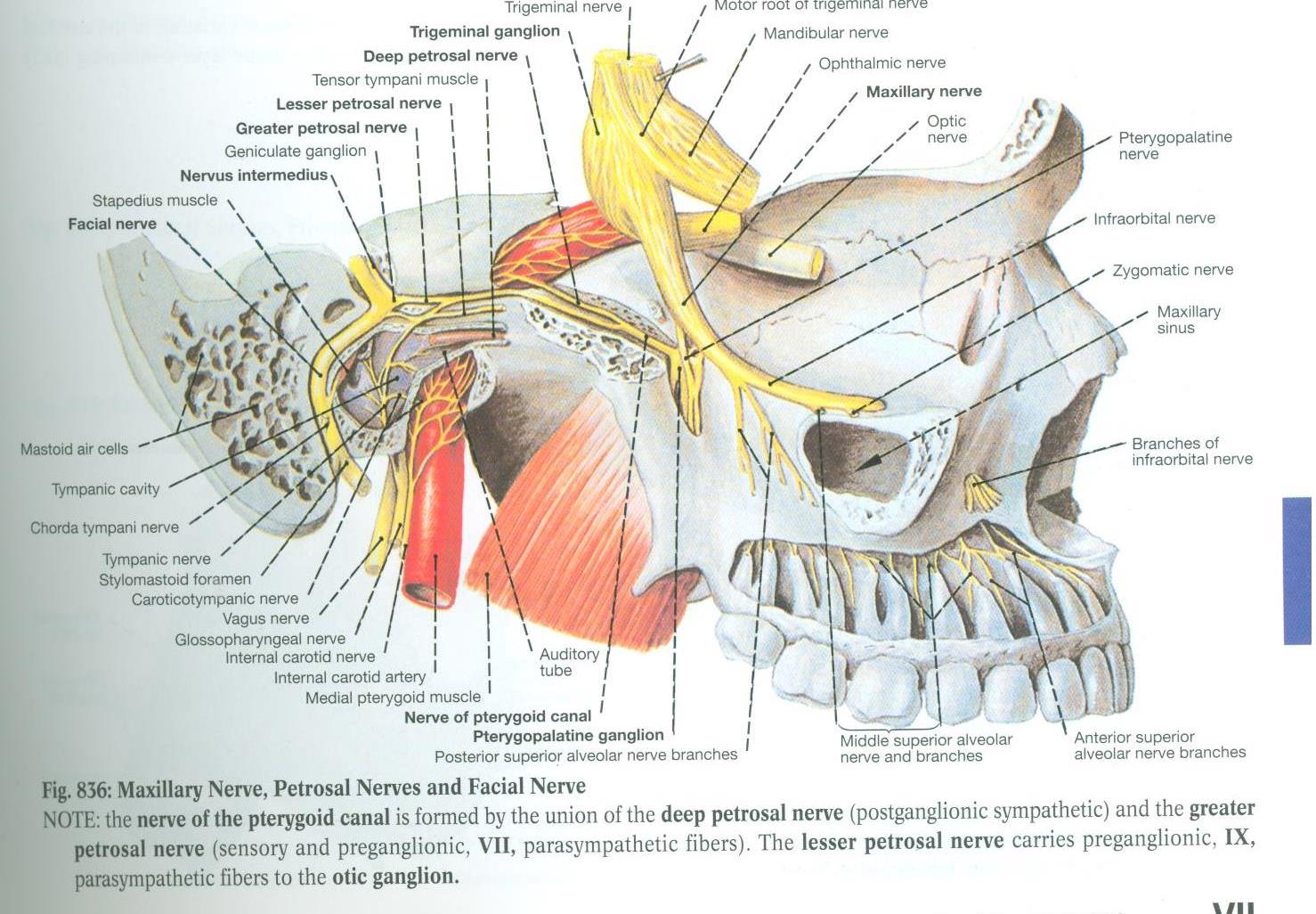
- Follow the greater palatine nerve and the lesser palatine nerve superiorly until they appear to converge. This is the inferior extent of the pterygopalatine ganglion (Fig. 7.86). The pterygopalatine ganglion is the location for synapse of preganglionic axons of the facial nerve (CN VII) that course first in the greater petrosal nerve and then in the nerve of the pterygoid canal (Vidian nerve). Postganglionic axons that arise in the pterygopalatine ganglion distribute with branches of the maxillary division of the trigeminal nerve (CN V2). The pterygopalatine ganglion stimulates secretion from the mucosa of the nasal cavity, paranasal sinuses, nasopharynx, roof of the mouth, and soft palate. The pterygopalatine ganglion also stimulates the lacrimal gland.
- The nerve of the pterygoid canal enters the pterygopalatine fossa from posteriorly. Identify the nerve of the pterygoid canal (Plate 527 and Fig. 836)
- Follow the nerve of the pterygoid canal anteriorly toward the pterygopalatine ganglion. The nerve of the pterygoid canal contains preganglionic parasympathetic axons from the greater petrosal nerve and postganglionic sympathetic axons from the deep petrosal nerve.
- Identify:
- Maxillary artery - courses deeply toward the pterygomaxillary fissure. Near the pterygomaxillary fissure the maxillary artery gives rise to the:
- Sphenopalatine artery - passes through the pterygopalatine fossa and then through the sphenopalatine foramen to enter the nasal cavity
- Descending palatine artery - enters the greater palatine canal where it was dissected from the medial side. Within the canal, the descending palatine artery splits into the greater and lesser palatine arteries.
- Infraorbital artery - passes through the inferior orbital fissure to enter the infraorbital canal and emerge on the face at the infraorbital foramen
- Maxillary division of the trigeminal nerve (CN V2) - courses from the foramen rotundum to the inferior orbital fissure. The maxillary division passes through the pterygopalatine fossa and gives off pterygopalatine branches that will form the greater and lesser palatine nerves.

PALATE AND THE PHARYNGEAL WALL
Learning Objectives:
- Describe the hard and soft palates.
- Identify the muscles associated with the soft palate.
- Describe the nerve supply to the muscles and mucosa of the hard and soft palates.
The palate forms the floor of the nasal cavity and the roof of the oral cavity. The palate consists of two portions: the hard palate forms the anterior two-thirds and the soft palate constitutes the posterior one-third. The palate is covered by nasal mucosa on its superior surface and oral mucosa on its inferior surface. Numerous mucous glands (palatine glands) are present on the oral surface of the palate.
The order of dissection will be as follows: The mucosal folds of the inner pharyngeal wall will be reviewed. The mucosa will be stripped from the inner surface of the pharynx and the muscles that constitute the inner longitudinal muscle layer will be examined. Muscles that move the soft palate will then be studied. The nerves and blood vessels of the palate will be identified.
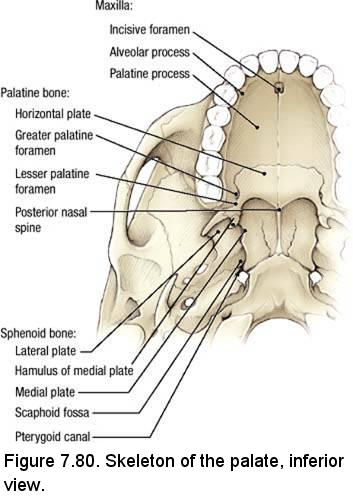
Osteology of the Hard Palate
Refer to a skull. From an inferior view, identify (Fig. 7.80): - Maxilla
- Incisive foramen
- Alveolar process
- Palatine process
- Palatine bone
- Horizontal plate
- Greater palatine foramen
- Lesser palatine foramina
- Posterior nasal spine
- Sphenoid bone
- Hamulus of the medial plate of the pterygoid process
- Medial plate of the pterygoid process
- Lateral plate of the pterygoid process
- Scaphoid fossa
- Pterygoid canal
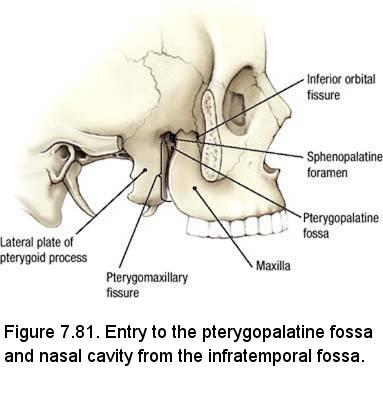
- Inferior orbital fissure
- Sphenopalatine foramen
- Pterygopalatine fossa
- Pterygomaxillary fissure
Dissection Instructions: Soft Palate
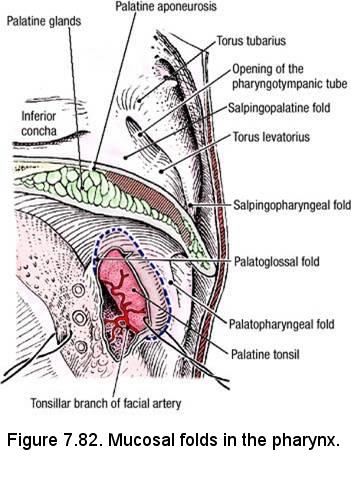
- Review the mucosal features of the inner pharyngeal wall (Fig. 7.82):
- Torus tubarius
- Opening of the pharyngotympanic tube
- Salpingopharyngeal fold
- Palatoglossal fold
- Palatopharyngeal fold
- Examine the edge of the soft palate where it is cut in the sagittal plane and observe (Fig. 7.82):
- The thickness of the soft palate is partly due to the presence of palatine glands.
- The strength of the soft palate is due to the palatine aponeurosis.
- The mobility of the soft palate is due to muscles that attach to its posterior two-thirds.
- Deep to the mucosa covering the palatopharyngeal fold are the delicate fibers of the palatopharyngeus muscle (Fig. 7.83). The superior attachments of the palatopharyngeus muscle are the hard palate and palatine aponeurosis and its inferior attachments are the thyroid cartilage and pharyngeal wall. The palatopharyngeus muscle elevates the larynx during swallowing.
- Deep to the mucosa covering the salpingopharyngeal fold are the delicate fibers of the salpingopharyngeus muscle (Fig. 7.83). The superior attachment of the salpingopharyngeus muscle is the cartilage of the pharyngotympanic tube. Its distal attachments and action are the same as the palatopharyngeus muscle, with which it blends. Note that the palatopharyngeus and salpingopharyngeus muscles contribute to the inner longitudinal muscle layer of the pharynx.
- The gap between the superior border of the superior pharyngeal constrictor muscle and the base of the skull is closed by the pharyngobasilar fascia. Passing through this gap are the pharyngotympanic tube and the levator veli palatini muscle (Fig. 7.83).
- The pharyngotympanic tube (auditory tube) connects the nasopharynx to the tympanic cavity. The part of the pharyngotympanic tube that is closest to the pharynx is cartilaginous (approximately two-thirds of its length) and the part that is closest to the middle ear passes through the temporal bone.
- Remove the mucosa inferior to the torus tubarius and identify the levator veli palatini muscle (Fig. 7.83). The superior attachments of the levator veli palatini muscle are the cartilage of the pharyngotympanic tube and the adjacent part of the temporal bone. Its distal attachment is the palatine aponeurosis. The levator veli palatini muscle elevates the soft palate.
- Remove the mucosa from the posterior border of the medial plate of the pterygoid process (Fig. 7.83) (just anterior to the levator veli palatini muscle). Identify the tensor veli palatini muscle, which lies lateral to the medial plate of the pterygoid process. The superior attachment of the tensor veli palatini muscle is the scaphoid fossa. The belly of the tensor veli palatini muscle is located between the medial and lateral plates of the pterygoid process. Its tendon turns medially around the hamulus of the medial pterygoid plate and forms the palatine aponeurosis. The tensor veli palatini muscle tenses the soft palate. Clean and identify the hamulus of the medial pterygoid plate and follow the tendon of the tensor veli palatini muscle around the hamulus of the medial pterygoid plate.
- Five muscles of the soft palate and pharynx are innervated by the vagus nerve (X) via the pharyngeal plexus: salpingopharyngeus, levator veli palatini, palatoglossus, palatopharyngeus, and musculus uvulae. The tensor veli palatini muscle is innervated by the mandibular division of the trigeminal nerve (V3).
- To remove the mucosa from the hard palate, use a probe to raise the mucosa on the inferior surface of the hard palate where it was cut during head bisection. Grasp the mucosa with forceps or a hemostat and use blunt dissection to peel it from medial to lateral.
- Identify the greater palatine nerve, artery and vein where they emerge from the greater palatine foramen (Fig. 7.84). Use blunt dissection to follow the greater palatine nerve anteriorly. Identify the nasopalatine nerve descending through the incisive canal from the nasal septum to supply the sensory innervation to the mucosa over the anterior part of the hard palate beyond the sensory field of the greater palatine nerve (Fig. 7.84).
- Posterior to the greater palatine nerve, identify the lesser palatine nerve and use blunt dissection to follow it towards the soft palate.


Dissection Instructions: Tonsilar Bed
Identify the palatine tonsil (Fig. 7.82).
- In older individuals, the palatine tonsil may be inconspicuous or may have been surgically removed. When present, the palatine tonsil is located in the tonsillar bed. Numerous invaginations of the mucosal epithelium form the openings into blind-ended tonsillar crypts. The boundaries of the tonsillar bed are:
- Anterior - palatoglossal fold
- Posterior - palatopharyngeal fold
- Lateral - superior pharyngeal constrictor muscle
- If the cadaver has a palatine tonsil, use blunt dissection to remove it (Fig. 7.82).
- Deep to the mucosa covering the palatoglossal fold are the delicate fibers of the palatoglossus muscle, which lies within the fold (Fig. 7.83). The superior attachment of the palatoglossus muscle is the palatine aponeurosis and its inferior attachment is the lateral side of the tongue. The palatoglossus muscle elevates the tongue and depresses the soft palate.
- The glossopharyngeal nerve (CN IX) passes between the superior and the middle pharyngeal constrictor muscles to enter the tonsillar bed. Remove the mucosa from the tonsillar bed and dissect the glossopharyngeal nerve to the root of the tongue (Fig. 7.83). The glossopharyngeal nerve innervates the mucosa of the posterior one-third of the tongue and the posterior wall of the pharynx.
- Near the glossopharyngeal nerve, identify the styloglossus muscle. Unlike the palatoglossus and palatopharyngeus muscles, which are sheet-like, the styloglossus muscle appears "blocky" like a pencil.
Dissection Review
- Return to the carotid triangle of the neck and follow the external carotid artery superiorly into the infratemporal fossa. Review the origin of the maxillary artery and its course through the infratemporal fossa. Review all branches of the maxillary artery that you dissected previously. Use an illustration to review the terminal branches of the maxillary artery (posterior superior alveolar, infraorbital, descending palatine, and sphenopalatine) and use the dissected specimen to review these branches where you have dissected them.
- Review the muscles that move the soft palate. State their attachments and actions.
- Review the pharyngeal wall, placing the pharyngeal constrictor muscles and the muscles of the soft palate into the correct muscle layers (inner longitudinal or outer circular).
- Review the pharyngeal plexus on the posterior surface of the pharynx and recall its role in innervation of the pharyngeal mucosa and the muscles of the pharynx and soft palate.
- Use the dissected specimen and an illustration to review the course of the glossopharyngeal nerve from the jugular foramen to the posterior one-third of the tongue.