THE BACK
Click
hyperlinks to go to the assigned dissection.
SURFACE ANATOMY ON THE CADAVER
DISSECTION
ASSIGNMENT: MONDAY, SEPTEMBER 14 – BACK I
DISSECTION
ASSIGNMENT: WEDNESDAY, SEPTEMBER 16 -BACK II
DISSECTION
ASSIGNMENT: MONDAY, SEPTEMBER 21 – BACK III
DISSECTION
ASSIGNMENT: TUESDAY, SEPTEMBER 22 – PECTORAL REGION I
DISSECTION
ASSIGNMENT: WEDNESAY, SEPTEMBER 23 – PECTORAL REGION II
The back
region contains the superficial muscles of the back, the intermediate
muscles of the back, and the deep muscles of the back. All of these
muscles attach to the vertebral column. The vertebral column serves the dual
purpose of forming the axis of the body and providing a protective bony
covering for the spinal cord.
Surface Anatomy on
the Cadaver
- Surface anatomy is studied on a living subject as part of your
assigned SURFACE ANATOMY exercises. You will be participating in surface
anatomy exercises on living subjects with your lab partners at another
time. In the cadaver, fixation may
make it difficult to distinguish bone from well-preserved soft tissues.
However, before beginning your dissection, you should make an effort to
palpate, or at least appreciate the general location of, specific anatomic
landmarks. Turn the cadaver to the
prone position (face down) and attempt to palpate the following structures
SURFACE
ANATOMY OF THE BACK
- External occipital protuberance
- Superior border of the trapezius muscle
- Spinous process of the seventh cervical vertebra (vertebra
prominens)
- Spine of the scapula (at vertebral
level T3)
- Acromion of the scapula
- Medial (vertebral) border of the scapula
- Inferior angle of the scapula (at vertebral
level T7)
- Spinous processes of thoracic vertebrae
- Erector spinae muscle (most noticeable
in the lumbar region)
- Median furrow
- Lateral border of the latissimus dorsi muscle (posterior axillary
fold)
- Iliac crest (at vertebral level L4)
- Posterior superior iliac spine
This
image shows musculature that are palpable structures in the back: PALPABLE
STRUCTURES IN THE BACK - MUSCULATURE
This
image shows bony prominences that are palpable structures in the back: PALPABLE
STRUCTURES IN THE BACK - BONY PROMINENCES
- Refer to a skeleton. On the scapula, identify SKELETON
OF THE BACK AND VERTEBRAL COLUMN
- Acromion
- Spine
- Superior angle
- Medial (vertebral) border
- Inferior angle
- On the ilium, identify:
- Iliac crest
- Posterior superior iliac spine
- On the occipital bone, identify:
- External occipital protuberance (inion)
- Superior nuchal line
- On the temporal bone, identify:
- Mastoid process
The vertebral
column consists of 33 vertebrae: 7 cervical (C), 12 thoracic (T), 5 lumbar
(L), 5 sacral (S), and 4 coccygeal (Co). The upper 24 vertebrae
(cervical, thoracic, and lumbar) allow flexibility and movement of the
vertebral column, whereas the sacral vertebrae are fused to provide rigid
support of the pelvic girdle. A typical thoracic vertebra will be described,
and the cervical and lumbar vertebrae will be compared to it.
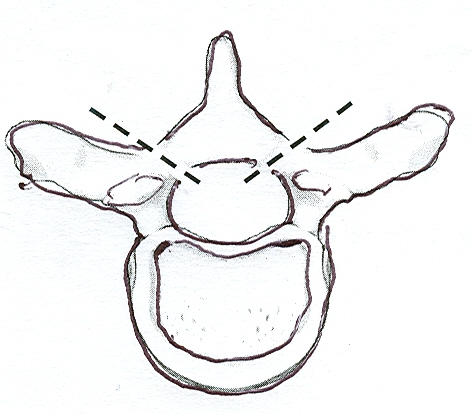
- Refer to a disarticulated thoracic vertebra and identify: TYPICAL
THORACIC VERTEBRA IN LATERAL AND SUPERIOR VIEWS
Body
- Vertebral arch – formed by the
combination of pedicles and laminae
- Pedicle (2 – the two here
indicates that there are two of them, right an left, per vertebra)
- Lamina (2)
- Vertebral foramen
- Transverse process (2)
- Transverse costal facet (2)
- Spinous process
- Articular processes – superior and inferior
(2 each)
- Articular facets – superior and inferior
(2 each)
- Vertebral notches – superior and inferior
(2 each)
- Costal facets – superior and inferior
(2 each)
- The spinous process of a thoracic vertebra is long, slender, and
directed inferiorly over the spinous process of the vertebra that is
inferior to it. Articulation with ribs is a characteristic of thoracic
vertebrae. The tubercle of a rib articulates with the transverse costal
facet of the thoracic vertebra of the same number (i.e., the tubercle of
rib 5 articulates with the transverse costal facet of vertebra T5). The
head of a rib articulates with the bodies of two adjacent vertebrae, (i.e.
the head of the rib articulates with the superior costal facet of the
vertebra of the same number and the inferior costal facet of the vertebra
superior to it). PART
OF THE THORACIC VERTEBRAL COLUMN
An intervertebral disc and the articular
processes unite two adjacent vertebrae. The vertebral notches of two
adjacent vertebrae combine to form an intervertebral foramen. A spinal
nerve passes through the intervertebral foramen.
- Cervical vertebrae differ from thoracic
vertebrae in the following ways: COMPARISON
OF CERVICAL, THORACIC, AND LUMBAR VERTEBRAE
Cervical
vertebrae have smaller bodies; larger vertebral foramina; shorter spinous
processes, which bifurcate at the tip; and transverse processes that contain a foramen transversarium. On a
disarticulated cervical vertebra and on an articulated skeleton, identify the
following features common to all cervical vertebrae:
- Transverse process
- Foramen transversarium
- Spinous process
Using a
disarticulated atlas and axis, and on an articulated skeleton, observe the
following features of individual cervical vertebrae:
- Atlas (C1) does not have a body.
- Axis (C2) has the dens, which is the body
of C1 that has become fused to C2 during development.
- Vertebra prominens (C7) has the most
prominent spinous process in the cervical region, hence its name.
- Lumbar vertebrae differ from thoracic
vertebrae in the following ways: COMPARISON
OF CERVICAL, THORACIC, AND LUMBAR VERTEBRAE
Lumbar vertebrae have larger bodies, have
broad spinous processes that project posteriorly, and do not have transverse
costal facets for ribs. On a skeleton, observe the lumbar vertebrae and notice
that their spines do not overlap like the spines of thoracic vertebrae.
The sacrum is formed by five
fused vertebrae and it does not have identifiable spines or transverse
processes. On the dorsal surface of the sacrum, identifySACRUM
AND COCCYX
- Median sacral crest
- Posterior (dorsal) sacral foramina
- Sacral hiatus
- The coccyx is a small triangular bone formed by four
rudimentary coccygeal vertebrae that are fused together.
TABLE: REGIONAL CHARACTERISTICS OF THE VERTEBRAE LINK
TABLE:
LIGAMENTS OF THE VERTEBRAL COLUMN LINK
Skin and Superficial Fascia
1.
Define
the "anatomical position". Using the conventional anatomical terms,
describe the body and the spatial relationships of its parts, for example
dorsal/ventral, medial/lateral, proximal/distal, and superficial/deep.
2.
Recognize
and define the standard planes and sections used to describe parts of the body
and the relationships of the various planes and sections to one another.
3.
Describe
the general structural plan of the body and the relationships of the layers,
partitions and compartments one encounters when dissecting from superficial to
deep in any particular region.
4.
Demonstrate
a cutaneous nerve and describe the pattern of cutaneous nerves on the back.
5.
Identify,
and give the general attachments of, nerve and blood supply to, and the general
functions of the superficial back muscles.
6.
Identify
the bony prominences of the back and spine that may be palpated and used for
reference to underlying structures.
7.
NOTE: FOR THIS AND ALL SUBSEQUENT DISSECTIONS you must be able to
identify any of the structures listed in the official course BODY PARTS LIST.
Dissection
Overview
The order
of dissection will be as follows: The skin will be reflected from the back,
posterior surface of the neck, and posterior surface of the proximal upper
limb. Posterior cutaneous nerves will be studied. The superficial fascia will
then be removed.
Dissection
Instructions
Skin
Incisions
- Refer to the following figure: SKIN
INCISIONS
- Use a scalpel to make a skin incision in the midline from the
external occipital protuberance (X) to the tip of the coccyx (S). The skin
is approximately 6 mm thick in this region.
- Make an incision from the tip of the coccyx (S) to the midaxillary
line (T). This incision should pass approximately 3 cm inferior to the
iliac crest.
- Make a transverse skin incision from the external occipital
protuberance (X) laterally to the base of the mastoid process (M).
- Make a transverse skin incision from R to B superior to the scapula
and superior to the acromion.
- At the level of the inferior angle of the scapula, make a
transverse skin incision from the midline (U) to the midaxillary line (V).
- To facilitate skinning, make several parallel transverse incisions
above and below the one described in the previous step. The strips of skin
that result should be about 7.5 cm wide to make skinning easier.
- Reflect the skin from medial to lateral, leaving the skin attached
laterally. On one side, reflect
only the skin, leaving the superficial fascia covering the muscles. On the other side, reflect the
superficial fascia with the skin.
Note that, after the dissection, the skin flaps can be placed back
over the deeper structures, serving to protect these underlying structures
from dessication.
Superficial
Fascia
- In the superficial fascia, locate the greater occipital nerve and
the occipital artery. GREATER
OCCIPITAL NERVE AND OCCIPITAL ARTERY
- The greater occipital nerve is the dorsal ramus of spinal nerve C2.
The greater occipital nerve pierces the trapezius muscle about 3 cm
inferolateral to the external occipital protuberance. The deep
fascia in this area is very dense and tough. It may be difficult to find
the greater occipital nerve by dissecting in this deep fascia, even though
it is a large nerve. Therefore, it
may be useful to cut the trapezius from the cervical spinous process and
nuchal ligament near the midline, enough to lift it slightly away from the
underlying semispinalis capitus muscle.
You may have to cut the trapezius from the superior nuchal line as
well. In this way, you should see
the greater occipital nerve passing through the semispanilis capitus and
the trapezius on its way to the skin.
The occipital artery may
be found lateral to the greater occipital nerve near the external
occipital protuberance. Note that
the occipital artery takes a superior-medial course as it passes from the
external carotid artery laterally toward the greater occipital
protuberance.
- A note about identifying arteries, nerves, and veins: Nerves are flat, solid, white, and
strong. Arteries are round, hollow,
and elastic. Veins are flat,
hollow, thin walled, and are often blue-black because they are filled with
coagulated blood. Larger structures
are readily distinguished in the dissection laboratory, and you will have
enough experience before the first exam that you can readily differentiate
these. Smaller structures make it
more difficult to differentiate these structures. However, note that, in many cases in
which the structures are too small to distinguish based on these physical
characteristics, you should still be able to make distinctions based on
anatomical relations that you are responsible for learning as part of the
dissection. In this case, if the greater
occipital nerve and occipital artery on your cadaver are too small to see
clearly which is which, you should easily distinguish between them because
the nerve is medial to the artery, and the nerve passes through the back
muscles as it makes its way to the skin over the skull, while the artery
arises from the lateral side of the neck and travels in a superior-medial
direction.
- Read a description of the dorsal ramus of a spinal nerve.
The posterior cutaneous branches of the dorsal rami pierce the
trapezius muscle or latissimus dorsi muscle to enter the superficial
fascia. BRANCHES
OF A TYPICAL SPINAL NERVE
- On the side where you did NOT reflect the superficial fascia with
the skin (i.e. the side where you left the superficial fascia covering the
back muscles), dissecting in the superficial fascia about 1-2 cm lateral
to the midline to find at least one representative of a dorsal ramus. Once you find at least one dorsal ramus,
go ahead and remove the remaining superficial fascia from the muscle.
- In the neck, reflect the superficial fascia
only as far laterally as the superior border of the trapezius muscle. Do
not cut the deep fascia along the superior border of the trapezius muscle.
The accessory nerve is superficial at this location and it is in danger of
being cut.
Dissection
Review
- Review the branching pattern of a typical spinal nerve and
understand that cutaneous branches of the dorsal rami innervate the skin
of the back.
- Study a dermatome chart and become familiar with the concept of
segmental innervation. SCHEMATIC
DEMARCATION OF DERMATOMES
Superficial Muscles of the Back
Dissection
Overview
The superficial
muscles of the back are the trapezius, latissimus dorsi, rhomboid
major, rhomboid minor, and levator scapulae. SUPERFICIAL
(EXTRINSIC) MUSCLES OF THE BACK
The order
of dissection will be as follows: The superficial surface of the trapezius
muscle will be cleaned. The trapezius muscle will be examined
and reflected. The latissimus dorsi muscle will be studied and reflected. The
rhomboid major muscle, rhomboid minor muscle, and levator scapulae muscle will
be studied. Dissection of the superficial back muscles should be performed
bilaterally.
Dissection Instructions
Trapezius Muscle
- Clean the surface of the trapezius muscle (L. Trapezoides,
an irregular four-sided figure). HOW
TO REFLECT THE MUSCLES OF THE BACK
- Do not disturb the
superior border of the trapezius muscle. Observe the proximal
attachment of the trapezius muscle on the external occipital protuberance,
the nuchal ligament, and the spinous processes of vertebrae C7 to T12.
- Observe the three parts of the trapezius muscle, each of which has
a distinctly different action:
- Superior part of the trapezius muscle
attaches to the lateral one-third of the clavicle; this portion elevates
the scapula.
- Middle part of the trapezius muscle
attaches to the acromion and spine of the scapula; this portion retracts
the scapula.
- Inferior part of the trapezius muscle
attaches near the medial end of the spine of the scapula; this portion
depresses the scapula.
- To reflect the trapezius muscle, insert your fingers deep to the
inferolateral border of the muscle (medial to the inferior angle of the
scapula). Use your fingers to break the plane of loose connective tissue
that lies between the trapezius muscle and the deeper muscles of the back.
- Use scissors to detach the trapezius muscle from its proximal
attachment on the spinous processes and the nuchal ligament (dashed
line on left side, near midline) HOW
TO REFLECT THE MUSCLES OF THE BACK Start inferiorly
and continue the cut superiorly as far as the external occipital
protuberance. Note that you may
already have completed this cut superiorly when you searched for the
greater occipital nerve.
- Use scissors to make a short transverse cut (2.5 cm) across the
superior end of the trapezius muscle to detach it from the superior nuchal
line. Spare the greater occipital nerve, and do not extend the
transverse cut beyond the border of the trapezius muscle.
- Use scissors to cut the trapezius muscle from its distal
attachments on the spine and acromion of the scapula (dashed line on
left side, near spine of scapula) HOW
TO REFLECT THE MUSCLES OF THE BACK Make this cut very
close to the bone. Leave the trapezius muscle attached to the clavicle and
cervical fascia.
- Reflect the trapezius muscle superolaterally. Leave the cervical
fascia attached along the superior border of the trapezius muscle to act
as a hinge.
- Study the deep surface of the reflected trapezius muscle. Find and
clean the plexus of nerves formed by the accessory nerve (cranial nerve
XI) and branches of the ventral rami of spinal nerves C3 and C4.
The accessory nerve provides motor innervation to the trapezius muscle;
the branches of nerves C3 and C4 are sensory (proprioception). Dissect the
superficial branch of the transverse cervical artery that
accompanies the nerves. Remove the transverse cervical vein to clear the
dissection field.
- The accessory nerve passes through the posterior triangle of the
neck. Do not follow the nerve into the posterior triangle at this time.
The posterior triangle will be dissected with the neck.
- Continuing our discussion about identifying arteries, nerves, and
veins: Your cadaver may be large
enough that the accessory nerve and superficial branch of the transverse
cervical artery are readily distinguished.
However, in some cadavers, they might be too small to differentiate
with certainty. In addition, they
both take a similar course anatomically (at least the anatomy you are
seeing right now; when we get to the neck, you will see that they do have
a different origin), For practical
exams, in cases where the structures are too small to distinguish and
there is no anatomical basis to differentiate them, we will indicate in
the question to “Identify the tagged nerve.” or “Identify the tagged
artery.” to prompt you toward the correct answer.
Latissimus Dorsi Muscle
- Clean the surface and define the borders of the latissimus dorsi
muscle (L. Latissimus, widest). HOW
TO REFLECT THE MUSCLES OF THE BACK
·
The proximal
attachments of the latissimus dorsi muscle are the spines of vertebrae T7 to
T12, the thoracolumbar fascia, and the iliac crest. The latissimus dorsi muscle
also has a proximal attachment to ribs 9 to 12, lateral to their angles.
·
Note that the distal attachment of the latissimus dorsi
muscle is the floor of the intertubercular sulcus on the anterior side of the
humerus, but do not dissect this attachment. The latissimus dorsi muscle
receives the thoracodorsal nerve and artery on its anterior surface near
its distal attachment; do not look for these structures now. The distal attachment of the latissimus dorsi
muscle, its nerve, and its artery will be dissected with the upper limb.
- To reflect the latissimus dorsi muscle, insert your fingers deep to
the superior border of the muscle (medial to the inferior angle of the scapula),
and break the plane of loose connective tissue that lies between it and
deeper structures. Raise the latissimus dorsi muscle enough to insert
scissors and cut through its proximal attachment on the thoracolumbar
fascia HOW
TO REFLECT THE MUSCLES OF THE BACK (dashed line on right side).
Do not cut too close to the lumbar spinous processes.
- Reflect the latissimus dorsi muscle laterally. Do not disturb its
attachment to the ribs. It may also have an attachment to the inferior
angle of the scapula. If so, do not disturb its attachment to the inferior
angle of the scapula.
The thoracolumbar fascia (lumbodorsal fascia)
THE
THORACOLUMBAR FASCIA is a deep investing membrane which covers the deep
muscles of the back of the trunk. It is made up of three layers, anterior,
middle, and posterior. The anterior layer is the thinnest and the posterior
layer is the thickest. Two spaces are formed between these three layers of the
fascia. Between the anterior and middle layer lies the quadratus lumborum
muscle. The erector spinae muscle is enclosed between the middle and posterior
layers.
Above, it passes in front of the serratus posterior
superior muscle and is continuous with a similar investing layer on the back of
the neck—the nuchal fascia.
In the thoracic region the lumbodorsal fascia is a thin
fibrous lamina which serves to bind down the Extensor muscles of the vertebral
column and to separate them from the muscles connecting the vertebral column to
the upper extremity. It contains both longitudinal and transverse fibers, and
is attached, medially, to the spinous processes of the thoracic vertebrae:
laterally to the angles of the ribs.
Rhomboid
Major and Rhomboid Minor Muscles
- Clean the surface and borders of the rhomboid (rhomboideus)
minor muscle and the rhomboid major muscle (Gr. Rhombos,
shaped like a kite). Typically, the separation between the rhomboid
muscles is not very obvious and the two muscles must be distinguished from
each other by using their distal attachments.
- The proximal attachments of the rhomboid minor muscle are the
nuchal ligament and the spinous processes of vertebrae C7 and T1. The
distal attachment of the rhomboid minor muscle is the medial border of the
scapula at the level of the spine.
- The proximal attachments of the rhomboid major muscle are the
spinous processes of vertebrae T2 to T5. The distal attachment of the
rhomboid major muscle is the medial border of the scapula inferior to the
spine.
- The rhomboid muscles retract the scapula, rotate the scapula to
depress the glenoid cavity, and hold the scapula close to the thoracic
wall.
- To reflect the rhomboid muscles, insert your fingers deep to the
inferior border of the rhomboid major muscle and separate it from deeper
muscles.
- Working from inferior to superior, use scissors to detach the
rhomboid major muscle from its proximal attachments on the spinous
processes. Continue the cut superiorly and detach the rhomboid minor
muscle from its proximal attachments on the spinous processes. Reflect
these two muscles laterally.
- Examine the deep surface of the two rhomboid muscles near their
distal attachments on the medial border of the scapula. Use blunt
dissection to find the dorsal scapular nerve and dorsal scapular
vessels. Remove the dorsal scapular vein to clear the dissection
field. The dorsal scapular nerve and artery course parallel to the medial
border of the scapula.
- The dorsal scapular artery may branch directly from the
subclavian artery, or it may arise from the transverse cervical artery, in
which case it is also called the deep branch of the transverse cervical
artery.
Levator Scapulae Muscle
- Identify the levator scapulae muscle (L. levare, to
raise). At this stage of the dissection, the levator scapulae muscle can
be seen only near its distal attachment on the scapula.
- Note that the proximal attachments of the levator scapulae muscle
are the transverse processes of the upper four cervical vertebrae. Do not
dissect its proximal attachments.
- The distal attachment of the levator scapulae muscle is the
superior angle of the scapula.
- The dorsal scapular nerve and artery supply the levator scapulae
muscle. The levator scapulae muscle elevates the scapula and rotates the
scapula to depress the glenoid cavity.
Dissection
Review
- Replace the superficial muscles of the back in their correct
anatomical positions.
- Use the dissected specimen to review the proximal attachment,
distal attachment, action, innervation, and blood supply of each muscle
that you have dissected.
- Review the movements that occur between the scapula and the thoracic
wall.
- Use an illustration to observe the origin of the transverse
cervical artery and the origin of the dorsal scapular artery. Observe two
triangles associated with the latissimus dorsi muscle: the triangle of
auscultation and the lumbar triangle. THE
LUMBAR TRIANGLE AND THE TRIANGLE OF AUSCULTATION
IN THE
CLINIC TRIANGLES
OF THE BACK
Triangles
of the Back
The triangle
of auscultation is bounded by the latissimus dorsi muscle, the trapezius muscle,
and the rhomboid major muscle. Within the triangle of auscultation, intercostal
space 6 has no overlying muscles. This area is particularly well suited for
auscultation (listening to sounds produced by thoracic organs, particularly the
lungs).
The lumbar
triangle is bounded by the latissimus dorsi muscle, the external oblique
muscle, and the iliac crest. The floor of the lumbar triangle is the internal
oblique muscle of the abdomen. On rare occasions, the lumbar triangle is the
site of a lumbar hernia.
WEDNESDAY, SEPTEMBER 16 -BACK II
Intermediate Muscles of the Back
SUPERFICIAL
AND INTERMEDIATE MUSCLES OF THE BACK
The intermediate
muscles of the back are the serratus posterior superior muscle and
the serratus posterior inferior muscle. The serratus posterior superior
and inferior muscles are very thin muscles, which may have been accidentally
reflected with the rhomboid muscles or the latissimus dorsi muscle. If you do
not see the serratus posterior muscles, look for them on the deep surface of
the reflected rhomboid muscles or the reflected latissimus dorsi muscle.
- The proximal attachments of the serratus posterior superior
muscle are the nuchal ligament and the spinous processes of vertebrae
C7 to T3. Its distal attachments are the superior borders of ribs 2 to 5,
lateral to their angles.
- The proximal attachments of the serratus posterior inferior
muscle are the spinous processes of vertebrae T11 to L2. Its distal
attachments are the inferior borders of ribs 9 to 12, lateral to their
angles.
- The serratus posterior muscles are respiratory muscles, and they
are innervated by intercostal nerves.
FOCUS QUESTIONS ANSWER
1. What are the names of the nerves that innervate the subcutaneous tissue
and skin?
2. What is the function of the investing fascia?
3. Between some muscles there is loose fascia, fat and connective tissue.
What is the function of this fascia?
4. Why do nerves, arteries, and veins branch in
different manners?
5. Where do nerves C3 and C4 (branching off of
anterior primary rami of spinal nerves) combine to form the subtrapezial
plexus?
6. What is the thoracolumbar fascia (aponeurosis)?
7. In reference to latissimus dorsi: How are the
costal attachments of the muscle related to adjacent muscles? Is there an
attachment to the scapula?
Deep Muscles of the Back and Spinal Cord
LEARNING
OBJECTIVES:
1.
Identify and give
the function of the significant parts of a typical vertebra and associated
ligaments.
2.
Identify the specialized
vertebrae.
3.
Describe the
spine, its curvatures, and vertebral column movements.
4.
Identify the
coverings and the supporting structures of the spinal cord. Give the point of
the termination of the spinal cord and the dural sac.
5.
Identify the
terminal specialties of the cord, their relation to lumbar puncture, the nerve
rootlets, and blood supply.
6.
Describe the
anatomy of the cord and vertebrae as related to fractures, dislocations, and
possible cord injury.
7.
Describe or
illustrate the location and function of the basic somatic motor and sensory
neurons on a cross section of the spinal cord (see Atlas+ or textbook).
8.
Describe a typical
spinal nerve, the somatic motor and sensory components found in any portion,
and their distribution.
9.
Describe
conceptually how any region of the thoracic wall gets its blood supply and
innervation.
10.
Define and explain
the significance of dermatomes.
11.
Explain the
difference between superficial and deep (true) back muscles.
Dissection
Overview
The deep muscles of the back DEEP
MUSCLES OF THE BACK act on the
vertebral column. There are many deep muscles of the back INTERMEDIATE
AND DEEP INTRINSIC BACK MUSCLES and only
a few will be dissected: splenius capitis muscle, splenius cervicis muscle,
semispinalis capitis muscle, and erector spinae muscle. All of the
deep muscles of the back are innervated by dorsal rami of spinal nerves.
The order
of dissection will be as follows: The deep muscles of the posterior neck (splenius
capitis and cervicis) will be studied and reflected. The semispinalis capitis
muscle will be studied. The erector spinae muscle will be dissected and the
three columns of muscle that comprise its component parts will be identified.
Dissection Instructions
Splenius Muscle
- Identify the splenius muscle (Gr. splenion, bandage).
- The splenius muscle lies deep to the trapezius muscle. The fibers
of the splenius muscle course obliquely across the neck. The proximal
attachment of the splenius muscle is the nuchal ligament and the spinous
processes of vertebrae C7 to T6.
- The splenius muscle has two parts that are named according to their
distal attachments:
- Splenius capitis muscle (L. caput,
head) is attached to the mastoid process of the temporal bone and the
superior nuchal line of the occipital bone.
- Splenius cervicis muscle (L. cervix,
neck) is attached to the transverse processes of vertebrae C1 to C4.
- The two parts of the splenius muscle are not easily distinguished
at this stage of the dissection. Detach both parts of the splenius muscle
from the nuchal ligament and the spinous processes of vertebrae C7 to T6.
- Reflect the muscles laterally, leaving their distal attachments
undisturbed.
Erector Spinae Muscle
- The erector spinae muscle (L. erector, one who
erects) lies deep to the serratus posterior muscles. DEEP
MUSCLES OF THE BACK
- Detach both serratus posterior muscles from their proximal
attachments on the spinous processes. Reflect the muscles laterally,
leaving them attached to the ribs.
- The erector spinae muscle is composed of three columns of muscle: spinalis, longissimus, and iliocostalis.
The intent of this dissection is to identify these three columns of
muscle.
- Use a scalpel to incise the posterior surface of the thoracolumbar
fascia. Use blunt dissection to remove it from the posterior surface
of the erector spinae muscle.
- Use your fingers to separate the three columns of muscle at
midthoracic levels. The columns of the erector spinae muscle are fused to
each other at the level of their inferior attachments to the sacrum and
ilium.
- Identify: DEEP
MUSCLES OF THE BACK
- Spinalis muscle – the medial column of
the erector spinae muscle. The inferior attachments of the spinalis
muscle are on spinous processes. Its superior attachments are also on
spinous processes. The spinalis muscle is present at lumbar, thoracic,
and cervical vertebral levels.
- Longissimus muscle (L. longissimus,
the longest) – the intermediate column of the erector spinae muscle. Its
inferior attachment is on the sacrum and its superior attachments are the
transverse processes of the thoracic and cervical vertebrae. Note that
its most superior portion, the longissimus capitis muscle,
attaches to the mastoid process of the temporal bone.
- Iliocostalis muscle – the lateral
column of the erector spinae muscle. Its inferior attachment is the ilium
(iliac crest) and its superior attachments are on ribs (L. costa,
rib).
- All three columns of the erector spinae muscle extend the vertebral
column when both sides work together. If only one side of the erector
spinae muscle is active, it bends the vertebral column laterally toward
the side that is active.
Transversospinal
Group of Muscles THE
TRANSVERSOSPINAL GROUP OF DEEP BACK MUSCLES
- The transversospinal group of muscles is located deep to the
erector spinae muscle. The muscles in the transversospinal group attach to
transverse processes and spinous processes. The muscles of the
transversospinal group cause rotational and lateral bending movements
between adjacent vertebrae and act to stabilize the vertebral column. A
number of muscles comprise this group: semispinalis, multifidus,
and more deeply, rotatores.
On one side, in the thoracic region, remove some of the fibers of
the spinalis muscle to expose muscles of the transversospinal group. You do not need to distinguish the semispanilis,
multifidus, and rotators specifically, just recognize them as the
transversospinal group of muscles.
Semispinalis Capitis Muscle
- The semispinalis fibers in the cervical region attach to the base
of the skull, and thus are specifically identified as the semispinalis capitis muscle.
- Identify the semispinalis capitis muscle (L. semi, half; L. spinalis,
spine). THE
SEMISPINALIS MUSCLES
- The semispinalis capitis
muscle is the most superficial member of the transversospinal group of
muscles. The semispinalis capitis muscle lies deep to the splenius muscles
and its fibers course vertically, parallel to the long axis of the neck.
- The inferior attachments of the semispinalis capitis muscle are the
transverse processes of the upper thoracic vertebrae.
- The superior attachment of the semispinalis capitis muscle is the
occipital bone between the superior and inferior nuchal lines. Note that
the greater occipital nerve passes through the semispinalis capitis
muscle.
- Do not dissect the semispinalis capitis muscle further at this
time.
IN THE CLINIC
Back
pain is a nonspecific term for pain from a variety of sources. It is
experienced by 80% of people during their lifetime and results from an upright
stance and a bipedal gait. A few of the many factors that can cause back pain
are dehydration and stiffening of the intervertebral disc with age,
osteoporosis of the zygapophysial joints between the veretebrae, and weakened
back and abdominal musculature, leading to poor posture.
TABLE:
INTRINSIC MUSCLES OF THE BACK (origin, insertions, actions) LINK
Dissection
Review
Use the
dissected specimen to review the location, innervation, and action of each
muscle or column of muscles in the deep group of back muscles.
Suboccipital Region
Dissection
Overview
First,
review the relevant osteology:
On a skull, identify: SKELETON
OF THE BACK, VERTEBRAL COLUMN, AND SKULL
- Superior nuchal line
- Inferior nuchal line
- External occipital protuberance
- Foramen magnum
- On the atlas (C1 vertebra), identify: POSTERIOR
VIEW OF ATLAS (C1) AND AXIS (c2)
- Posterior tubercle
- Posterior arch
- Groove for the vertebral artery
- Transverse process
- Foramen transversarium
On the axis (C2 vertebra),
identify: POSTERIOR
VIEW OF ATLAS (C1) AND AXIX (C2)
- Spinous process
- Transverse process
- Foramen transversarium
The order
of dissection will be as follows: The greater occipital nerve will be
identified and followed deeply. The semispinalis capitis muscle will be
reflected. The muscles that bound the suboccipital triangle will be identified.
The contents of the suboccipital region (vertebral artery and suboccipital
nerve) will be studied. All dissections
will be done bilaterally, with the exception of the vertebral artery, whick
will be dissected on one side only.
Dissection
Instructions
- Identify the semispinalis capitis muscle. THE
SUBOCCIPITAL REGION
- Once again, find the greater occipital nerve. Use blunt dissection
to follow the greater occipital nerve deeply, through the semispinalis
capitis muscle. Detach the semispinalis capitis muscle close to the
occipital bone and reflect it inferiorly. Preserve the greater occipital
nerve.
- Deep to the semispinalis capitis muscle, follow the greater
occipital nerve proximally to the lower border of the obliquus capitis
inferior muscle. Note that the greater occipital nerve (dorsal ramus
of C2) emerges between vertebrae C1 and C2.
- Identify and clean the three muscles that form the boundaries of
the suboccipital triangle: CONTENTS
OF THE SUBOCCIPITAL TRIANGLE
- Obliquus capitis inferior muscle (inferior oblique muscle) forms
the inferior boundary of the suboccipital triangle. Verify that the
proximal attachment of the obliquus capitis inferior muscle is the
spinous process of the axis (C2). Its distal attachment is on the
transverse process of the atlas (C1).
- Rectus capitis posterior major muscle (rectus major muscle) forms the medial boundary of the suboccipital triangle. Confirm
that the proximal attachment of the rectus capitis posterior major muscle
is the spinous process of the axis. Its distal attachment is the inferior
nuchal line of the occipital bone.
- Obliquus capitis superior muscle (superior oblique muscle) forms the lateral boundary of the suboccipital triangle. Confirm
that the inferior attachment of the obliquus capitis superior muscle is
the transverse process of the atlas. Its superior attachment is the
occipital bone between the superior and inferior nuchal lines.
- The muscles that bound the suboccipital triangle produce extension
and lateral bending of the head at the atlanto-occipital joints and
rotation of the head at the atlantoaxial joints.
- The contents of the suboccipital triangle are the suboccipital
nerve and the vertebral artery. CONTENTS
OF THE SUBOCCIPITAL TRIANGLE Note that the
suboccipital nerve (dorsal ramus of C1) emerges between the occipital bone
and vertebra C1. The suboccipital nerve supplies motor innervation to the
muscles of the suboccipital region. The suboccipital nerve is the only dorsal
ramus that has no cutaneous distribution.
Dissect the fascia within the borders of the suboccipital triangle
to find the main trunk and branches of the suboccipital nerve.
- Determine which side has the better dissection of the muscles of
the suboccipital triangle and the suboccipital nerve, and identify the vertebral
artery on the other side. To do so, use the muscles of the
suboccipital triangle and finger palpation to identify the posterior arch
of the atlas. Then, remove the
muscles of the suboccipital triangle, taking care not to cut deep to the
posterior arch of the atlas. Use
blunt dissection to identify the vertebral artery coursing along the
superior border of the posterior arch of the atlas. Remove the vertebral vein if
necessary. Once the artery is
identified, trace it laterally to the transverse foramen of the
atlas. Use blunt dissection to find
the artery as it courses between the transverse foramina of the atlas and
axis.
- Use an illustration to study the course of the vertebral artery
through the neck and into the skull.
TABLE: MUSCLES OF THE SUBOCCIPITAL REGION (origin,
insertion, action) LINK
Dissection
Review
- Review the actions of the suboccipital muscles. THE
SHORT SUBOCCIPITAL (NUCHAL) MUSCLES
- Review the distribution of the branches of a thoracic dorsal ramus
and compare the thoracic pattern to the distribution of the dorsal rami of
spinal nerves C1 to C3.
FOCUS QUESTIONS ANSWER
1. Describe the anatomy of the cord and vertebrae as related to
fractures, dislocations, and possible cord injury.
2. Describe or illustrate the location and function of the basic somatic
motor and sensory neurons on a cross section of the spinal cord.
3. Describe a typical spinal nerve, the somatic motor and sensory
components found in any portion, and their distribution.
4. Describe conceptually how any region of the thoracic wall gets its
blood supply and innervation.
5. Define and explain the significance of dermatomes.
6. Explain the difference between superficial and true back muscles.
MONDAY, SEPTEMBER 21 – BACK III
Vertebral Canal, Spinal Cord, and Meninges
Dissection
Overview
The vertebral canal is a bony
tube formed by the stacked vertebral foramina of the cervical
vertebrae, thoracic vertebrae, lumbar vertebrae, and sacral
canal. THE
SPINAL CORD WITHIN THE VERTEBRAL CANAL The vertebral canal encloses and protects the spinal
cord, its membranes (spinal meninges), and blood vessels. The spinal
cord begins at the foramen magnum of the occipital bone and usually terminates
in the adult at the level of the second lumbar vertebra. Because the spinal
cord is shorter than the vertebral canal, the spinal cord segments are found
at higher vertebral levels than their names would suggest.
The spinal cord is not uniform in
diameter throughout its length. It has a cervical enlargement THE
CERVICAL AND LUMBAR ENLARGEMENTS that corresponds to spinal cord segments C4
to T1 and a lumbar enlargement that corresponds to spinal cord segments
L2 to S3. There are 31 pairs of spinal nerves (8 cervical, 12 thoracic,
5 lumbar, 5 sacral, and 1 coccygeal), which emerge between adjacent vertebrae.
Most spinal nerves are numbered according to the vertebra above them as they
pass through the intervertebral foramen (i.e., spinal nerve T1 exits the
vertebral canal below vertebra T1). However, in the cervical region, spinal
nerves are numbered differently—they are numbered according to the vertebra
below. For example, spinal nerve C1 exits the vertebral canal above vertebra C1
and the C8 spinal nerve, which does not have a correspondingly numbered
vertebra exits between vertebra C7 and T1.
The order
of dissection will be as follows: The erector spinae muscles will be removed
from the lower back to expose the laminae of the vertebrae. The laminae will
then be cut and removed (laminectomy) to expose the spinal meninges. The spinal
meninges will be examined and will be opened to expose the spinal cord. The
spinal cord will then be studied.
Dissection Instructions
|
- Attempt to keep as much of the lamina intact as possible during
removal. The dura mater will remain
with the spinal cord and will be undamaged.
- On the deep surface of the removed spinous specimen, gently remove
any adherent epidural fat to expose the ligamenta flava. The
ligamenta flava connect the laminae of adjacent vertebrae.
Spinal
Meninges
- Observe the epidural (extradural) space. Use blunt
dissection to remove the epidural fat and the posterior internal
vertebral venous plexus from the epidural space.
- Identify the dural sac, which ends inferiorly at vertebral
level S2LOWER
PORTION OF THE VERTEBRAL CANAL AND SPINAL CORD. A. LATERAL VIEW. B.
POSTERIOR VIEW In the thoracic region, lift a fold of dura
mater with forceps and use scissors to cut a small opening in its
dorsal midline. Use scissors to extend the cut inferiorly to vertebral
level S2. Attempt to do this without damaging the underlying arachnoid
mater. Retract the dura mater and pin it open.
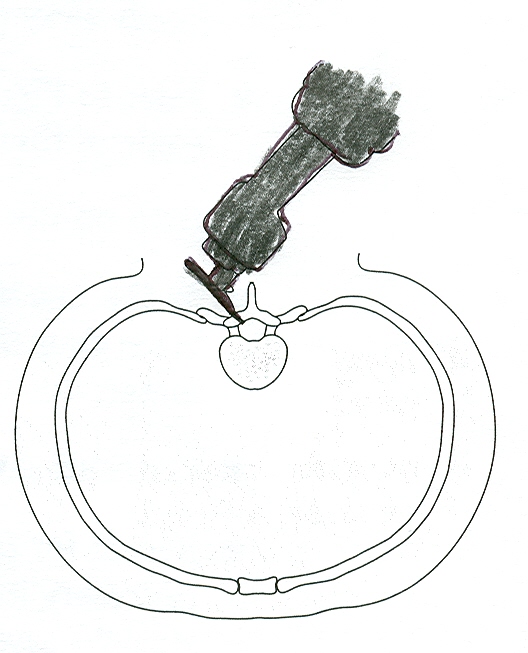
- Identify the arachnoid mater. RELATIONSHIPS
OF THE MENINGES TO THE SPINAL CORD AND NERVE ROOTS. A. TRANSVERSE SECTION.
B. POSTERIOR VIEW. It is very delicate.
Incise the arachnoid mater in the dorsal midline and observe the subarachnoid
space. The subarachnoid space contains cerebrospinal fluid in the
living person but not in the cadaver.
- Retract the arachnoid mater and observe the spinal cord. The
spinal cord is completely invested by pia mater, which is on the
surface of the spinal cord and cannot be dissected from it.
- Identify the following features of the spinal cord:
- Cervical enlargement (spinal cord
segments C4 to T1) provides nerves to the upper limb.
- Lumbar enlargement (spinal cord segments
L2 to S3) provides nerves to the lower limb. The lumbar enlargement is
located at lower thoracic vertebral levels.
- Conus medullaris (medullary cone) is the end of the spinal cord located between vertebral levels L1
and L2.
- Cauda equina (L., tail of horse) is a
collection of ventral and dorsal roots in the lower vertebral canal. LOWER
PORTION OF THE VERTEBRAL CANAL AND SPINAL CORD
- Filum terminale internum is a delicate filament continuous with
the pia mater. It arises from the
inferior tip of the conus medullaris and ends at S2, where it is encircled
by the lower end of the dural sac.
- Filum terminale externum (coccygeal ligament) is the continuation
of the filum terminale internum below vertebral level S2. The filum
terminale externum passes through the sacral hiatus and ends by attaching
to the coccyx. You will not see the
filum terminal externum on your cadaver.
- The pia mater forms two denticulate ligaments, one on each
side of the spinal cord. RELATIONSHIP
OF THE MENINGES TO THE SPINAL CORD AND NERVE ROOTS Each denticulate ligament
has 21 teeth and each tooth is attached to the inner surface of the dura
mater, anchoring the spinal cord.
- Use a probe to follow dorsal roots and ventral roots
to the point where they pierce the dura mater and enter the intervertebral
foramen. DISSECTION
OF A DORSAL ROOT GANGLION The dorsal roots are on the
dorsal side of the denticulate ligament and the ventral roots are on the
ventral side of the denticulate ligament. The spinal nerve will be formed
outside of the vertebral canal at the point where the dorsal and ventral
roots join each other.
- Observe small blood vessels that course along the ventral
and dorsal roots. These are branches of posterior intercostal, lumbar, or
vertebral arteries, (depending upon vertebral level) that pass into the
vertebral canal through the intervertebral foramen and supply the spinal
cord.
- In the thoracic region, expose one spinal nerve. Place a
probe into an intervertebral foramen to protect the nerve within it (i.e.
place the probe between the bone and exiting nerve roots). Use bone
cutters to remove the posterior wall of the intervertebral foramen, and
then use blunt dissection to expose the spinal ganglion (dorsal
root ganglion). DISSECTION
SHOWING DORSAL AND VENTRAL ROOTS OF A SPINAL NERVE Distal to the spinal ganglion, identify
the spinal nerve and follow it distally to the point where it divides into
a dorsal ramus and a ventral ramus.
IN THE
CLINIC
Vertebral
Venous Plexuses
The veins
of the vertebral venous plexuses are valveless, permitting blood to flow
superiorly or inferiorly, depending on blood pressure gradients. The vertebral
venous plexuses can serve as routes for metastasis of cancer from the pelvis to
the vertebrae, vertebral canal, and cranial cavity.
IN THE
CLINIC
Lumbar
Puncture
Cerebrospinal fluid (CSF) can be
obtained from the subarachnoid space inferior to the conus medullaris. LINK
At this level, there is no danger of
penetrating the spinal cord with the puncture needle.
Dissection
Review
- Review the formation and branches of a typical spinal nerve.
- Describe the way that the deep back muscles receive their
innervation.
- Review the coverings and parts of the spinal cord and study an
illustration that shows the blood supply to the spinal cord.
- Consult a dermatome chart and relate this pattern of cutaneous
innervation to the spinal cord segments.
FOCUS QUESTIONS ANSWER
1. What is the coccygeal ligament?
2. What do the lateral continuities of the dura mater cover at and
distal to the intervertebral foramen?
3. What does the subarachnoid space usually contain?
4. With what is the subarachnoid space continuous?
5. Where does the filum terminale lie?
6. Where does the filum terminale attach?
8.What are the relations of the denticulations and the denticulate
ligament to the roots of spinal nerves?
8. How many denticulations are there?
9. Where do the denticulations attach?
10. At what vertebral level is the conus medullaris?
11. Where is the dura mater in relation to the intervertebral foramen?
12. Examine dorsal and ventral rootlets as they emerge from the cord.
How is the segmental pattern created?
13. What is a root?
14. What is the functional difference between dorsal and ventral roots?
15. Trace the roots to the point of union to form the spinal nerve. Are
they in separate sheaths before uniting?
16. Where is the dorsal root ganglion?
17. Note posterior and anterior spinal arteries. What are their sources?
18. What reinforces the spinal arteries?
19. What are radicular arteries?
20. Are all radicular arteries the same?
21. What is the source for radicular arteries?
22. Observe arrangement of gray matter and white matter of the cord.
What is their significance?
23. After exposing the posterior longitudinal ligament in cervical and
lumbar regions, can you see the intervertebral discs?
24. What is the significance of the attachment of the posterior
longitudinal ligament to the discs?
TUESDAY, SEPTEMBER 22 – PECTORAL
REGION I
THE PECTORAL REGION
Dissection
Overview
The pectoral
region (L., pectus, chest) covers the anterior thoracic wall and
part of the lateral thoracic wall. The order of dissection will be as follows:
The breast will be dissected in female cadavers. The superficial fascia will be
removed in cadavers of both sexes. The superficial fascia of the thorax
contains the usual elements that are common to superficial fascia in all body
regions: blood vessels, lymph vessels, cutaneous nerves, and sweat glands. In
addition, the superficial fascia of the anterior thoracic wall in the female
contains the mammary glands, which are highly specialized organs unique to the
superficial fascia of the thorax.
Surface
Anatomy and Osteology
The
surface anatomy of the pectoral region will be studied on a living subject as
part of your SURFACE ANATOMY assigned exercises. You can also observe some of
the anatomy on the cadaver. At this point we will only consider anatomy
relevant to our dissection of the pectoral region. A more detailed study of the
osteology of the thorax will be undertaken during our dissection of the thorax
in Block II. Turn the cadaver to the supine position and palpate the following
structures: SURFACE
ANATOMY OF THE ANTERIOR THORACIC WALL
- Clavicle
- Acromion of the scapula
- Manubrium
- Body of the sternum
- Xiphoid process
- Seventh costal cartilage
- Costal margin
Skeleton
of the Thorax
Refer to
a skeleton. Examine a rib from the midthorax level and identify: TYPICAL
LEFT RIB, POSTERIOR VIEW
- Head
- Neck
- Tubercle
- Costal angle
- Shaft (body)
- Costal groove
Examine
the sternum and identify: SURFACE
ANATOMY OF THE ANTERIOR THORACIC WALL
- Manubrium (L. manubrium,
handle)
- Body
- Xiphoid process (Gr. xiphos,
sword)
Examine a
scapula and identify: SCAPULA,
ANTERIOR VIEW
- Acromion
- Coracoid process
Observe
that the medial end of the clavicle articulates with the manubrium of
the sternum (sternoclavicular joint) and the lateral end of the clavicle
articulates with the acromion of the scapula (acromioclavicular joint): ARTICULATIONS
OF THE SCAPULA
Dissection
Instructions
Skin
Incisions
- Refer to Figure SKIN
INCISIONS FOR THE ANTERIOR THORACIC REGION
- Use a sharp scalpel to make a midline incision
from the jugular notch (A) to the xiphosternal junction (C).
- Make transverse incision from the jugular
notch (A) along the clavicle to the acromion (B). Extend this cut to a point just beyond
the shoulder (F).
- Make a transverse incision from the
xiphosternal junction (C) along the costal margin, to the midaxillary line
(V).
- Make a transverse incision through the nipple,
from the sternum to the midaxillary line.
An additional transverse incision from the sternum to the
midaxillary line may be useful to aid in reflection of the skin.
- DO NOT make a vertical lateral incision (G-V),
or the circular incision around the arm (G-F), because these would result
in removal of the skin.
- Starting near the midline, reflect each flap
of skin and superficial fascia from medial to lateral; the plane of
dissection should be between the superficial fascia of the skin and the
deep fascia of the pectoralis major muscle. Just lateral to the sternum, take note
of any anterior cutaneous branches of the intercostal nerves
and anterior intercostal vessels as they are ligated.
- Reflect the skin just a little ways into the
upper limb. We will dissect the
upper limb in the winter quarter.
Stay away from the deep structures of the axilla, especially the brachial
plexus.
- Near the midaxillary line, pull the skin and
superficial fascia laterally, teasing apart the connective tissue with
your fingers until you find at least one representative of a lateral
cutaneous branch of an intercostal nerve, and accompanying
branches of the posterior intercostal vessels, as they leave the
intercostal space to supply the skin of the lateral wall of the thorax.
- Between the lateral thoracic wall and the
axilla, find one named lateral cutaneous branch of an intercostal nerve,
the intercostobrachial nerve, which is the lateral cutaneous branch
of T2 and, therefore, will exit between ribs 2 and 3 on its way to the
skin of the axilla and medial side of the arm. Thus the nerve has clinical importance
because of its association with referred pain of a heart attack.
Look in the superficial
fascia near the clavicle for fibers of the platysma muscle. This very thin muscle of facial expression
will be dissected in more detail when we study the head and neck in the
spring. Any fibers of the platysma
muscle may be reflected superiorly to accommodate further dissection of the
thorax
Breast
The
breast is dissected in female cadavers only. Students with male cadavers must
observe at another dissection table. Because of the advanced age of some
cadavers, it may be difficult to dissect and identify all of the structures
listed. Expect the lobes of the gland to be replaced by fat with advanced age.
The breast
extends from the lateral border of the sternum to the midaxillary line, and
from rib 2 to rib 6. The mammary gland is a modified sweat gland that is
contained within the superficial fascia of the breast. THE
BREAST IN SAGITTAL SECTION The
breast is positioned anterior to the pectoral fascia (the deep fascia of
the pectoralis major muscle). The pectoral fascia is attached to the overlying
skin by the suspensory ligaments of the breast that pass between the
lobes of the mammary gland.
- Identify the areola and the nipple. THE
BREAST IN SAGITTAL SECTION
- If not already done so during the reflection of the skin flaps, use
a sharp scalpel blade to divide the mammary gland into two halves. The cut can be made in any orientation,
but should pass through the nipple.
Do not extend your cut deep into the underlying pectoral fascia and
pectoralis major muscle.
- Examine the cut surface of the breast, and use the handle of a
forceps to scoop the fat out of several compartments between suspensory
ligaments. These areas between suspensory ligaments once contained
lobes of functional glandular tissue.
- Find and clean one of the 15 to 20 lactiferous ducts that
converge on the nipple. Identify the lactiferous sinus, which is an
expanded part of the lactiferous duct located deep to the nipple.
- Note that in most cadavers, it will be difficult to distinguish the
lactiferous ducts from the suspensory ligaments based on their individual
physical appearance. The easiest
way to distinguish lactiferous ducts from suspensory ligaments is that the
lactiferous ducts converge on the nipple, while most of the suspensory
ligaments connect to other areas of the skin of the breast.
- Trace one lactiferous duct to the nipple and attempt to identify
its opening.
- Use an illustration to study the lymphatic drainage of the
mammary gland.
- Insert your fingers behind the breast and open the retromammary
space. This is the plane you used for reflection of the skin. Note that the normal breast can be
easily separated from the underlying deep fascia of the pectoralis major
muscle.
IN THE
CLINIC
Breast
For
descriptive purposes, clinicians divide the breast into four quadrants. The
superolateral (upper outer) quadrant contains a large amount of glandular
tissue and is a common site for breast cancers to develop. From this quadrant,
an “axillary tail” of breast tissue often extends into the axilla.
In
advanced stages of breast cancer, the tumor may invade the underlying
pectoralis major muscle and its fascia. When this happens, the tumor and breast
become fused to the chest wall, a condition that can be detected by palpation
during a physical examination. As the breast tumor enlarges, it places traction
on the suspensory ligaments, resulting in dimpling of the skin overlying the
tumor.
Dissection
Review
- Review the location and parts of the breast.
- Use an illustration to review the vascular supply to the breast.
- Discuss the pattern of lymphatic drainage of the breast and
identify by name the lymph node groups that are involved.
- Use an illustration of the branching pattern of a typical spinal
nerve to review the innervation of the anterior thoracic wall and breast. DISTRIBUTION
OF A THORACIC SPINAL NERVE
WEDNESDAY, SEPTEMBER 23 –
PECTORAL REGION II
Muscles of the Pectoral Region
Dissection
Overview
The muscles
of the pectoral region are the pectoralis major, pectoralis minor, and
subclavius muscles. The muscles of the pectoral region attach the upper limb to
the thoracic skeleton. The pectoral muscles are positioned immediately deep to
the superficial fascia (deep to the breast).
The
dissection will proceed as follows: The pectoralis major muscle will be studied
and reflected. The pectoralis minor muscle and clavipectoral fascia will be
studied. The subclavius muscle will be identified. The pectoralis minor muscle
will be reflected, and the branches of the thoracoacromial artery will be
dissected.
Dissection
Instructions
- Clean the superficial surface of the pectoralis major muscle,
using your fingers to define its borders CUTS FOR REFLECTION OF THE PECTORALIS
MAJOR AND PECTORALIS MINOR MUSCLES Study an illustration
and note that the deep fascia on the surface of the pectoralis major
muscle is called pectoral fascia and that it is continuous with the
axillary fascia that forms the floor of the axilla.
- Identify the two heads of the pectoralis major muscle: clavicular
head and sternocostal head. Observe
that the juncture of these two heads is at the sternoclavicular joint.
- Use your fingers to trace the tendon of the pectoralis major muscle
to its distal attachment on the humerus. The pectoralis major muscle
flexes, adducts, and medially rotates the humerus.
- Between the clavicular head of the pectoralis major muscle and the
adjacent deltoid muscle, use blunt dissection to define the borders of the
deltopectoral triangle and find the cephalic vein. Preserve
the cephalic vein in subsequent steps of this dissection. Note that variation in venous structures
is quite common; therefore the cephalic veins on your cadaver may be large
or small, and are often not bilaterally symmetrical.
- Relax the sternal head of the pectoralis major muscle by flexing
and adducting the arm. Gently insert your fingers posterior to the
inferior border of the pectoralis major muscle. Create a space between the
posterior surface of the pectoralis major and the clavipectoral fascia.
Push your fingers superiorly to open this space.
- Use scissors to detach the sternoscostal head of the pectoralis
major muscle from its attachment to the sternum (CUTS
FOR REFLECTION OF THE PECTORALIS MAJOR AND PECTORALIS MINOR MUSCLES,
dashed line on right side).
- Palpate the deep surface of the pectoralis major muscle to locate
the medial and lateral pectoral nerves and vessels. Preserve these
nerves and vessels.
- Use scissors to cut the clavicular head of the pectoralis major
muscle close to the clavicle.
- Preserve the cephalic vein. Gently reflect the pectoralis major
muscle laterally, noting that the lateral pectoral nerve and the pectoral
branch of the thoracoacromial artery enter the deep surface of the
clavicular head. Do NOT damage
these structures.
- Deep to the pectoralis major muscle are the clavipectoral fascia,
pectoralis minor muscle, and subclavius muscle.
- Identify the pectoralis minor muscle. The proximal attachment of
the pectoralis minor muscle is ribs 3 to 5 near their costal cartilages.
Its distal attachment is the coracoid process of the scapula. The
pectoralis minor muscle draws the glenoid cavity of the scapula anteriorly
and inferiorly.
- Note that the medial pectoral nerve pierces the pectoralis
minor muscle and then enters the pectoralis major muscle, innervating
both, while the lateral pectoral nerve (and the thoracoacromial artery)
passes through the clavipectoral fascia superior to the pectoralis minor
muscle, and thus innervates only the pectoralis major muscle.
- Identify the subclavius muscle, which is located inferior to
the clavicle MUSCLES
IN THE PECTORAL REGION. The subclavius muscle, which is attached
to the clavicle and the first rib, depresses the clavicle.
- Read a description of the clavipectoral fascia and
understand that it is immediately deep to the pectoralis major muscle. The
clavipectoral fascia is attached to the clavicle. It passes both
superficial and deep to the subclavius muscle and the pectoralis minor
muscle. The clavipectoral fascia is attached to the axillary fascia
inferiorly.
- Clean the cephalic vein where it crosses the anterior
surface of the pectoralis minor tendon. The cephalic vein passes through
the clavipectoral fascia medial to the pectoralis minor tendon.
- Use scissors to detach the pectoralis minor muscle from its
proximal attachments on ribs 3 to 5 (CUTS
FOR REFLECTION OF THE PECTORALIS MAJOR AND PECTORALIS MINOR MUSCLES,
dashed line on left side).
- Reflect the pectoralis minor muscle superiorly. Leave the muscle
attached to the coracoid process of the scapula.
- Clean and define the branches of the thoracoacromial artery BLOOD
SUPPLY TO THE PECTORAL REGION :
- Acromial branch passes laterally across
the coracoid process toward the acromion.
- Deltoid branch courses laterally in
the deltopectoral groove between the deltoid muscle and pectoralis
major muscle. The deltoid branch accompanies the cephalic vein.
- Pectoral branch passes between the
pectoralis major muscle and the pectoralis minor muscle and supplies
both.
- Clavicular branch courses superiorly and
medially to supply the subclavius muscle.
- Note that you will NOT be required to name these branches
specifically, just be able to identify the main thoracoacromial artery.
- Also note that the thoracoacromial artery, and the lateral and
medial and pectoral nerves, may be difficult to differentiate, especially
if they are small. To make the
distinction clear, dissect the thoracoacromial artery posteriorly until
you see it branching from the large axillary
artery. Clean out a small
region of the axillary artery to positively identify it, removing any
small veins that obscure the dissection field. Note that the lateral pectoral nerve arises
from the brachial plexus of nerves (to be dissected later), and here is
seen passing superior-lateral to the axillary artery. The medial pectoral nerve passes
medial-inferior to the axillary artery.
- Along the lateral border of the pectoralis minor muscle, identify
the lateral thoracic artery. This vessel arises from the axillary
artery near the origin and at right angles to the thoracoacromial artery,
and passes inferiorly toward the thoracic cage.
- Identify the serratus anterior muscle MUSCLES
OF THE PECTORAL REGION. Note its extensive proximal attachment
on the upper eight ribs. The distal attachment of the serratus anterior
muscle is the deep surface of the scapula along the entire length of its
medial border. You cannot see the distal attachment at this time. Find the innervation of the serratus
anterior muscle, the long thoracic
nerve, which arises from the brachial plexus and runs inferiorly on
the lateral surface this muscle.
Dissection
Review
- Replace the pectoral muscles into their correct anatomical
positions.
- Review the attachments of the pectoralis major, pectoralis minor,
and subclavius muscles. Review their actions, innervations, and blood
supply.
- Review the relationship of the clavipectoral fascia to the muscles,
vessels, and nerves of this region.
- Be sure that you understand the role played by the clavipectoral
fascia in supporting the floor of the axilla.
FOCUS QUESTIONS ANSWER
1. From where do the lateral cutaneous branches (anterior and posterior)
of intercostal nerves arise and to where do they distribute?
2. Is any pinkish mammary glandular tissue visible?
3. What are suspensory ligaments of the mammary glands?
4. Consider blood supply, nerve supply, and lymphatic drainage of the
breasts.
5. Why are lateral and medial pectoral nerves reversed (with respect to
their names and relative locations) from what you would expect? 6. Where does
the cephalic vein terminate?
 A
A
 B
B
 C
C